Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Uveitis, psoriasis and inflammatory bowel disease (IBD) are common in axial spondyloarthritis (axSpA) but data on their impact on activity of musculoskeletal manifestations and functional status, in general, are contradictory. The aim of this study was to assess the impact of uveitis, psoriasis, and IBD on disease activity and functional status in a population-based cohort of patients with axSpA.
Methods: A stratified random sample of patients with axSpA (ICD-10 M45) was drawn from health insurance data in Germany. Patients in the sample received a survey on demographic, socioeconomic, and disease-related parameters including history of uveitis, psoriasis, and IBD.
Survey data were linked to health insurance data gathering additional information on recent/current occurrence (within one year) of uveitis, psoriasis, and IBD as well as drug prescriptions and non-pharmacological treatment.
Differences between patients with and without uveitis, psoriasis, and IBD were assessed. Separate multivariable linear regression models were calculated to determine the effect of uveitis, psoriasis, and IBD on disease activity and functional impairment after adjustment for other relevant parameters including treatment.
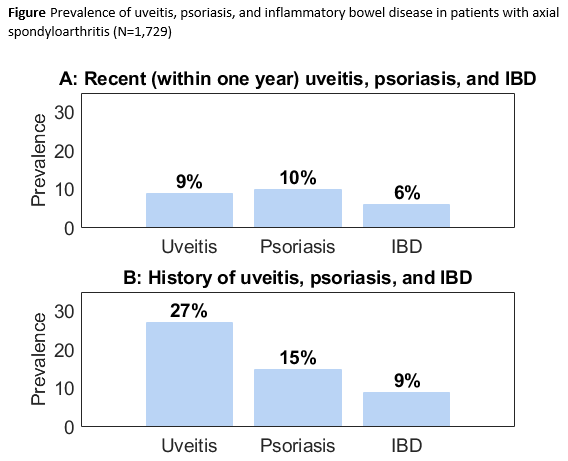
Results: A total of 1,729 patients with axSpA were included in the analyses. The patients’ main characteristics are shown in Table 1: The mean age was 55.9 years and 46.1% were female. The prevalence for recent (ever) uveitis, psoriasis, and IBD is illustrated in Figure: 9% (27%) of the patients had recently (ever) uveitis, 10% (15%) had recently (ever) psoriasis, and 6% (9%) had recently (ever) IBD. In 1.6% (6.9%) of the patients two of these conditions were recently (ever) present, and in 0% (0.5%) of the patients, all three conditions were recently (ever) present.
Results from the multivariable linear regression analyses are presented in Table 2 and revealed that history of psoriasis was significantly associated with both higher level of disease activity and higher level of functional impairment. History of IBD was also associated with higher disease activity, whereas recent psoriasis or IBD showed no strong association with disease activity and functional status.
In contrast, history of uveitis showed no strong association with disease activity and functional status while recent uveitis was significantly associated with lower disease activity according to the BASDAI even after adjustment for treatment.
Conclusion: Disease activity and functional impairment are higher in axSpA patients with a history of psoriasis or IBD, whereas history of uveitis does not have a major impact on activity of musculoskeletal manifestations and functional status in axSpA. However, recent uveitis showed a somewhat unexpected association with lower disease activity. The latter might be related to a higher likelihood of being treated with TNF inhibitors in the presence of uveitis.
To cite this abstract in AMA style:
Redeker I, Callhoff J, Hoffmann F, Haibel H, Sieper J, Zink A, Poddubnyy D. Is There an Impact of Uveitis, Psoriasis and Inflammatory Bowel Disease on Musculoskeletal Disease Activity and Function in Axial Spondyloarthritis? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/is-there-an-impact-of-uveitis-psoriasis-and-inflammatory-bowel-disease-on-musculoskeletal-disease-activity-and-function-in-axial-spondyloarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-there-an-impact-of-uveitis-psoriasis-and-inflammatory-bowel-disease-on-musculoskeletal-disease-activity-and-function-in-axial-spondyloarthritis/