Session Information
Date: Sunday, November 13, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: The majority of patients with PsA present with skin manifestations first. Several studies have examined the relationship between activity/severity of skin and joint manifestations, but the results have been variable. The objectives are to assess the association between the extent and severity of skin psoriasis and musculoskeletal manifestations of PsA at baseline and over time.
Methods: This is a retrospective analysis of a single centre inception cohort of patients enrolled in a tertiary care clinic from 2000-2020. Patients are assessed according to a standard protocol which records demographic information, the results of clinical skin and joint assessments and laboratory evaluations at 6–12-month intervals. Skin activity is measured by the PASI score, and joint disease activity is measured by the number of tender and swollen joints. Axial disease is measured by the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Bath Ankylosing Spondylitis Metrology Index (BASMI). Spearman correlations were calculated between PASI scores and joint counts and BASMI (in patients with axial disease). Multivariable analysis was carried out using negative binomial regression models for the joint counts and linear models for BASMI and BASDAI scores.
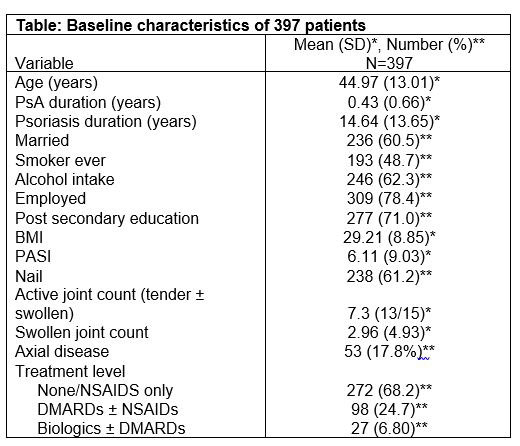
Results: The characteristics of 397 patients were enrolled within 12 months of PsA diagnosis are given in the table. A significant correlation was found between PASI score and the total active joint count (AJC) (ρ 0.024, p=0.01). Among patients on no treatment or NSAIDs at the baseline assessment, a one-unit PASI score reduction was associated with a 2.4% reduction of AJC when controlling for sex, age and psoriasis duration. There was no evidence of an association between PASI score and AJC in patients taking conventional DMARDs (cDMARDs), while for those receiving biologic DMARDs (bDMARDs) a one-unit decrease in PASI was associated with a 3.9% reduction in AJC. When all longitudinal data were considered, in the absence of DMARDs, AJC was reduced by 4.8% on average with a PASI decrease of 1. cDMARDs use did not demonstrate a correlation between PASI and AJC, while treatment with bDMARDs showed that for each decrease of PASI of 1, the AJC decreased by 4.4% on average. There was no association between the BASDAI score and the PASI score either at baseline or longitudinally. When adjusting for sex, age, and PsC duration, we found a positive association between PASI and BASMI scores in all treatment groups at baseline. The longitudinal analysis showed that PASI is positively associated with BASMI among patients on cDMARDs. Among patients with axial disease, a positive association was found between PASI and BASMI at baseline in all treatment groups except cDMARDs; a positive association was found between longitudinal PASI and BASMI scores in all treatment groups.
Conclusion: In patients presenting within 12 months of diagnosis of PsA, there is an association between the severity of skin and joint or axial disease, both at baseline and longitudinally, but the nature of the association differs according to medication use.
To cite this abstract in AMA style:
Gladman D, Aldabie G, Ma F, Sutton M, Lee K, Cook R. Is There a Correlation Between Skin and Musculoskeletal Activity in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/is-there-a-correlation-between-skin-and-musculoskeletal-activity-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-there-a-correlation-between-skin-and-musculoskeletal-activity-in-psoriatic-arthritis/