Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: The SARS-CoV-2 pandemic is a worldwide mental health crisis. We evaluated perceived stress in patients seeking care for musculoskeletal conditions, and explored associations with disease diagnoses and other sociodemographic factors.
Methods: A web-based survey was sent March 5, 2021 to 7505 subjects who had previously agreed to participate in our longitudinal COVID-19 registry. All were ≥ age 18 and had been evaluated at least once by a rheumatologist between April 1, 2018 and April 1, 2020 at a single Division of Rheumatology in New York City. ICD-10-CM algorithms were used to identify those with and without a systemic rheumatic disease (SRD). The Perceived Stress Scale (PSS), a widely used self-report instrument, evaluates how overloaded and uncontrollable subjects find their lives: 0-13 = low stress, 14-26=moderate stress and 27-40 = high stress. Subjects were designated as having had COVID-19 if they reported a positive SARS-CoV-2 PCR or antigen test or were diagnosed with COVID-19 by a medical provider. Descriptive statistics were calculated and p-values from Chi-square, T-test, ANOVA and Wilcoxon rank sum tests reported as appropriate.
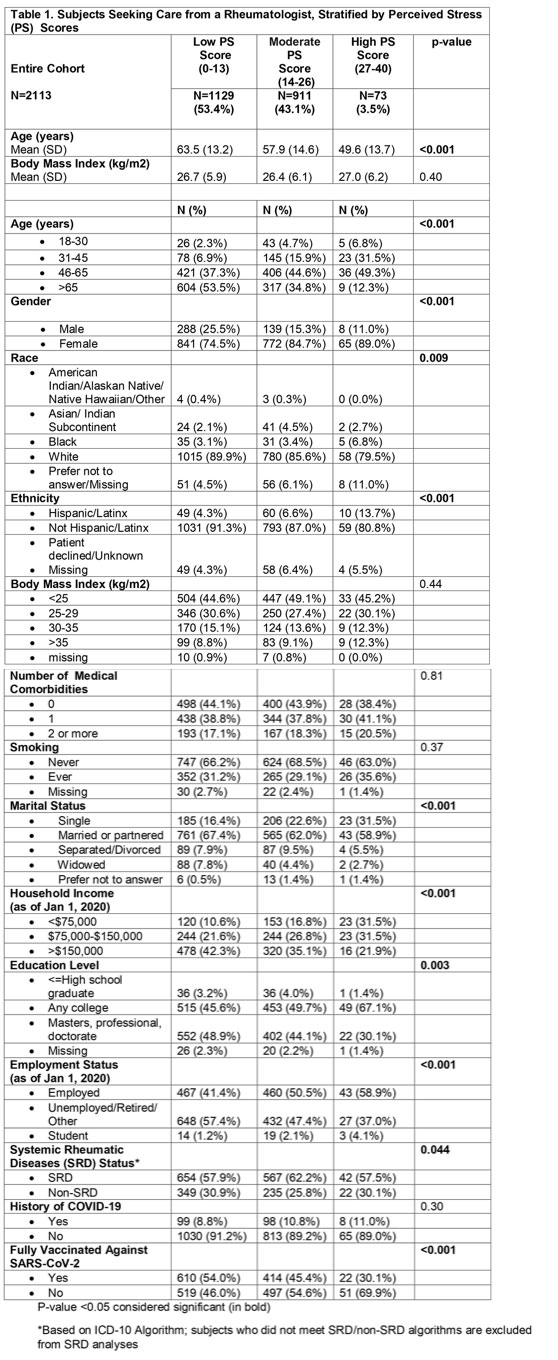
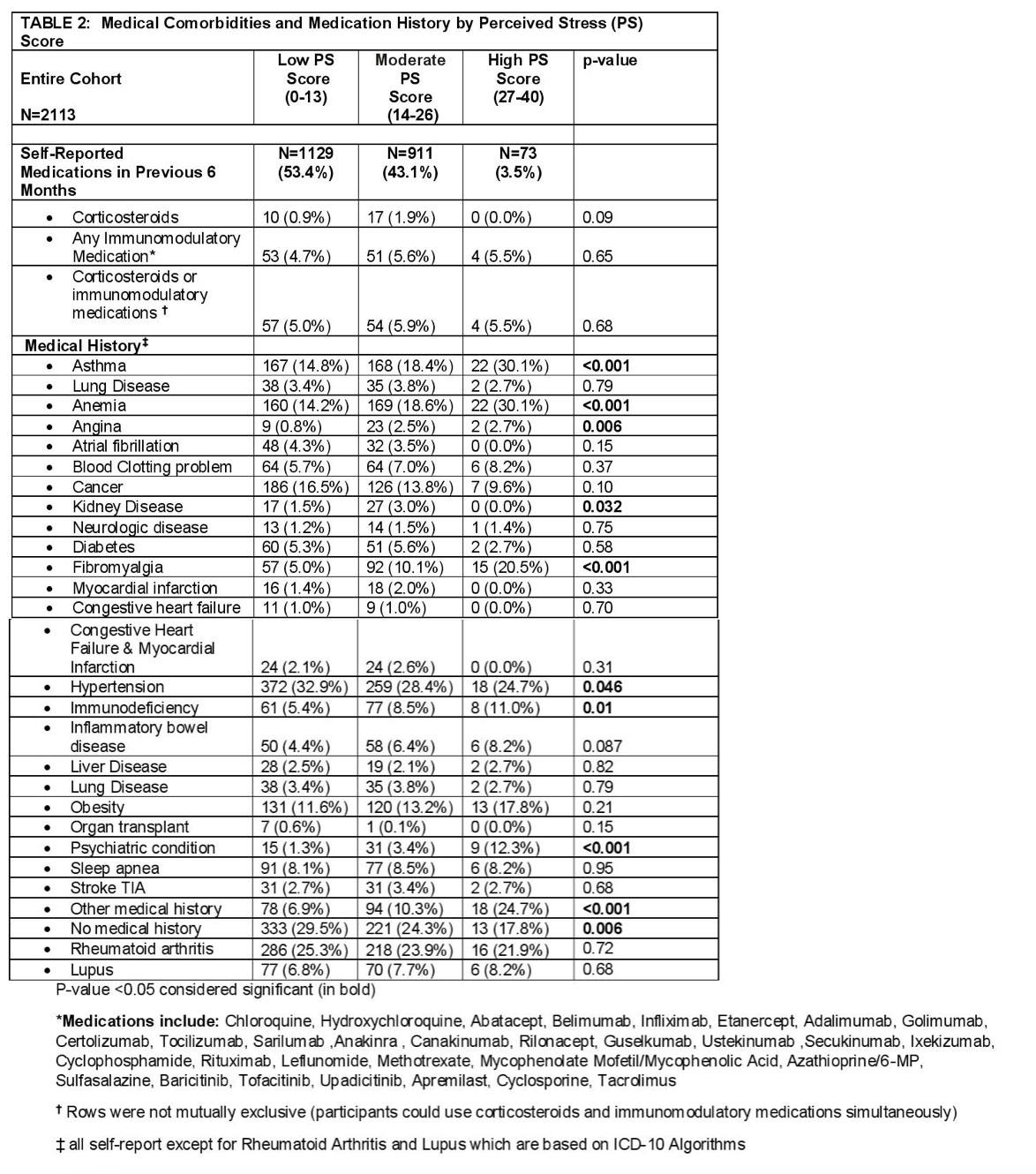
Results: 5977 (80%) responded to the “Wellness and Stress” section of the survey and 2113 (28.2%) completed the PSS. Mean age decreased with increasing perceived stress category (63.5 vs. 57.9 vs. 49.6 years; p< 0.001). < 1% of subjects over 65 years reported high perceived stress. Women were more likely than men to have high perceived stress, (p< 0.001) with double the percentage in the high PSS category, (3.87% vs.1.84%). Those reporting Black race, Hispanic/LatinX ethnicity, income < $75,000, being single, not being fully vaccinated against COVID-19, or having fibromyalgia, psychiatric conditions, anemia, angina or asthma were more likely to be in the highest perceived stress category, (p< 0.001). Those reporting no medical conditions or being employed were more likely to be in the lowest PSS category, (p= 0.006 and p< 0.001, respectively). There was no significant association between having had COVID-19 and PSS scores. Those with an SRD had higher perceived stress scores than non-SRD (p=0.044).
Conclusion: Among patients seeking care from a rheumatologist, an SRD diagnosis and other sociodemographic and medical factors were significantly associated with perceived stress, whereas a COVID-19 diagnosis was not. Women and those < 45 years old were more likely to report high PSS. Future multivariate regression analyses should evaluate whether PSS trends change over the course of the pandemic, as well as the association of perceived stress and long COVID.
To cite this abstract in AMA style:
Levine J, Barbhaiya M, Bykerk V, Jannat-Khah, DrPH, MSPH D, Mandl L. Is Perceived Stress Associated with COVID-19 or Having a Systemic Rheumatic Disease? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/is-perceived-stress-associated-with-covid-19-or-having-a-systemic-rheumatic-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-perceived-stress-associated-with-covid-19-or-having-a-systemic-rheumatic-disease/