Session Information
Date: Sunday, November 5, 2017
Title: Rheumatoid Arthritis – Human Etiology and Pathogenesis Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In a recent publication in Science Translational Medicine, Konig et al. (2016) describe a potential explanation for the link between periodontal infection and RA. They identify a specific periodontitis-associated bacterium: Aggregatibacter actinomycetemcomitans (Aa), which via its pore-forming toxin (leukotoxin A: LtxA) can dysregulate the activity of citrullinating enzymes in neutrophils. Furthermore, the authors report that the risk conferred by the most important genetic risk factor for RA: the HLA-DRB1 shared epitope (HLA SE) alleles, was limited to RA patients who had been exposed to Aa as determined by seropositivity to LtxA. Aiming to replicate their findings, we focused on two main questions: 1) is the increased exposure to Aa as measured by the presence of anti-LtxA-antibodies specific for RA, or also present in other forms of inflammatory arthritis? 2) can we replicate the finding that the association between HLA SE alleles and ACPA-positive RA is limited to the anti-LtxA-positive subset?
Methods: We established an ELISA against purified LtxA (acquired from the same source as in the original article) and tested sera from 594 patients from the Leiden Early Arthritis Clinic with various diagnoses, including RA, OA, SpA, PsA, sarcoidosis, and gout. Serial dilutions of a mix of 3 strongly positive RA patients were used as a standard, and the lowest point of the linear part of the standard curve (2000 AU/ml) was defined as the cut-off.
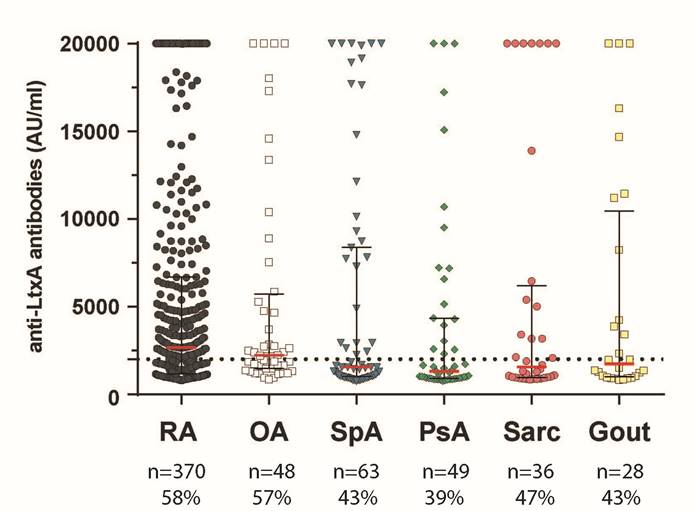
Results: As shown in Figure 1, anti-LtxA antibodies could be found in a substantial proportion of RA patients, but also in patients with other forms of arthritis. Within RA patients, there was no association with the presence of HLA SE alleles and/or ACPA, in contrast to the previous findings.
Conclusion: Although microbial influences may well be important in the development of RA, our results do not support a key role of exposure to LtxA originating from the periodontal pathogen Aa in linking the effect of the HLA SE alleles and periodontal disease to anti-citrullinated protein autoimmunity in RA.
Figure 1.
Distribution of anti-LtxA antibodies in sera of 594 patients suffering from early arthritis. Levels of anti-LtxA antibodies in the serum of each individual are shown.
LtxA Leukotxin A, RA Rheumatoid arthritis, Aa Aggregatibacter actinomycetemcomitans, OA Inflammatory osteoarthritis, SpA Spondylarthritis with peripheral arthritis, PsA Psoriatic arthritis, Sarc Sarcoidosis, ACPA anti-citrullinated protein antibodies, SE shared epitope. Red lines indicate the median level per group. The dashed line indicates the cut-off. The number of patients per group and percentage of patients positive according to the cut-off are shown underneath.
Reference:
M. F. Konig, L. Abusleme, J. Reinholdt, R. et al, Aggregatibacter actinomycetemcomitans–induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci. Transl. Med. 8, 369ra176 (2016).
To cite this abstract in AMA style:
Volkov M, Dekkers J, Loos BG, Bizzarro S, Huizinga TWJ, Praetorius HA, Toes REM, van der Woude D. Is Leukotoxin_A Produced By Aggregatibacter Actynomycetemcomitans Important for Initiating Autoimmune Responses Underlying Rheumatoid Arthritis? [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/is-leukotoxin_a-produced-by-aggregatibacter-actynomycetemcomitans-important-for-initiating-autoimmune-responses-underlying-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-leukotoxin_a-produced-by-aggregatibacter-actynomycetemcomitans-important-for-initiating-autoimmune-responses-underlying-rheumatoid-arthritis/