Session Information
Date: Wednesday, November 16, 2016
Title: Health Services Research II
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: About 50% of persons with knee OA are obese. Quality-adjusted life-year losses due to knee OA and obesity exceed 3.5 per person. The results of the Intensive Diet and Exercise for Arthritis (IDEA) trial showed that an intensive diet and exercise (D+E) program, consisting of meal replacements and group exercise sessions led by a professional exercise interventionist, led to a mean 10.6 kg weight reduction and 50% reduction in pain over 18 months. We sought to determine the cost-effectiveness of the D+E program in overweight and obese (BMI>27 kg/m2) OA patients.
Methods: We combined the data from the IDEA trial with the Osteoarthritis Policy (OAPol) Model, a validated computer simulation of knee OA, to evaluate long-term clinical and economic outcomes in knee OA patients similar to those enrolled in the IDEA trial. Mean age was 66, average WOMAC score 32 (0-100, 100 worst) and average BMI 33.6 kg/m2. We evaluated the cost-effectiveness of adding a D+E regimen to clinical management consisting of intermittent analgesia until patients are eligible and willing to have TKR. D+E efficacy and sustainability over 18 months were derived from IDEA and assessed on two domains: BMI reduction and pain reduction. 29% of subjects in D+E arm of IDEA trial had a BMI reduction between 5-10% and 8% reached a reduction of 20-25%. The discontinuation rate was estimated at 8% per year. Annual costs for the D+E regimen included costs of program ($328 in year 1, $281 in subsequent years), meal replacements during the first six months ($790) and a hypothetical (the trial subjects did not have to pay for it) gym membership ($600/year). The base-case analysis assumed maximum duration of efficacy to be 15 years. We adopted a modified societal perspective (without productivity costs), discounted outcomes at 3%/year, and assumed a willingness to pay (WTP) threshold of $100,000 per quality adjusted life year (QALY). Strategies with incremental cost-effectiveness ratios (ICERs) below WTP were considered cost-effective. We conducted sensitivity analyses on the inclusion of productivity costs, duration of efficacy and discontinuation rates. 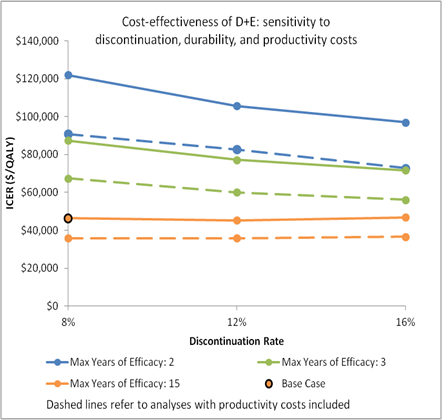
Results: In the base case, those who were offered the D+E regimen spent 7.4 years on the regimen, on average. They spent 2.9 years with at least 5% BMI reduction. The D+E regimen led to 12.4 quality-adjusted years of life gained per every 100 participants, resulting in an incremental cost-effectiveness ratio of $46,300/QALY. Inclusion of productivity costs decreased the ICER for the D+E regimen to $35,800. Reducing the duration of efficacy to 3 years increased the ICER for the D+E regimen to $87,400/QALY when productivity costs were not included ($67,500/QALY with productivity costs). (Figure)
Conclusion: Adding D+E to clinical management of overweight and obese patients with knee OA is cost-effective. Implementation of D+E into care of OA patients should be a public health priority.
To cite this abstract in AMA style:
Losina E, Smith KC, Paltiel AD, Suter LG, Katz JN, Messier SP. Is an Intensive Diet and Exercise Regimen Cost-Effective for Obese and Overweight Patients with Symptomatic Knee OA? [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/is-an-intensive-diet-and-exercise-regimen-cost-effective-for-obese-and-overweight-patients-with-symptomatic-knee-oa/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-an-intensive-diet-and-exercise-regimen-cost-effective-for-obese-and-overweight-patients-with-symptomatic-knee-oa/
