Session Information
Date: Wednesday, October 24, 2018
Title: 6W011 ACR Abstract: Spondyloarthritis Incl PsA–Clinical VI: Imaging of Axial SpA (2922–2927)
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Axial inflammation is a key feature in axial spondyloarthritis (axSpA). An (overall) definition of bone marrow oedema (BMO) on the MRI of the SIJ (MRI-SIJ) has been proposed by ASAS (i.e. considering all 8 anatomical quadrants (Q) of both SIJ together). This study aims to investigate how BMO evolves over time at the quadrant level by comparing several patterns of inflammation and their possible impact on clinical and structural outcomes.
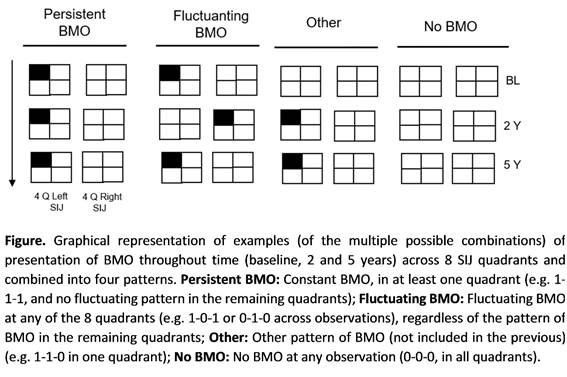
Methods: Patients from the DESIR cohort (early axSpA according to the rheumatologist) with MRI-SIJ available at baseline, 2 and 5 years were included. Each image was scored by 3 trained central readers blinded to chronological order. BMO was considered positive if detected (by ≥2/3 readers) in ≥1/6 slices in each of the 8 quadrants and per timepoint. Four different patterns of BMO throughout time were defined (persistent same Q BMO, persistent fluctuating Q BMO, other pattern of BMO and no BMO) considering all 8 quadrants (Figure). The four groups were compared in terms of clinical and imaging outcomes at 5 years.
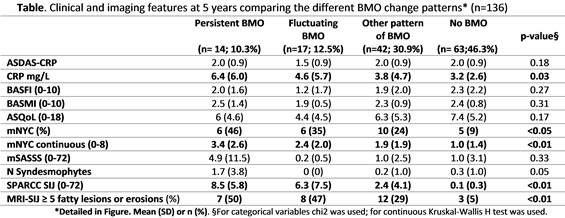
Results: In total 136 patients were included (age 34 (SD 9) years, 50% male, and 63% HLA-B27 positive). The ‘No BMO’ pattern was the most frequent (n=63; 46%). The fluctuating pattern was seen in 17 patients (13%) and the ‘persistent BMO’ in 14 patients (10%). ‘Other patterns of BMO’ (not fitting any of the previous) were seen in 42 patients (31%). Considering the increasing sequence of local inflammation as ‘no BMO’, ‘other patterns of BMO’, ‘fluctuating BMO’ and ‘persistent BMO’, a gradient could be found in several outcomes, namely: higher likelihood to be mNYC positive (9%, 24%, 35% and 46%, respectively); higher CRP (3.2, 3.8, 4.6 and 6.4 mg/L), higher SPARCC-SIJ scores (0.1, 2.4, 6.3 and 8.5), and a higher frequency of SIJ structural changes (≥5 fatty lesions or erosions: 5%, 29%,47% and 50%) at 5 years (Table). Bone formation was especially observed in the persistent BMO group. No differences in treatment were found across the groups.
Conclusion: Only 10% of the patients showed persistent inflammation in the same Q over a 5-year period and 12.5% fluctuating inflammation in different Qs. A gradient of higher structural damage and systemic inflammation was found in patients with increasing cumulative local inflammation at the quadrant level of the SIJ.
To cite this abstract in AMA style:
Rodrigues Manica S, Sepriano A, Ramiro S, Landewé RBM, Claudepierre P, Moltó A, Dougados M, van Lunteren M, van der Heijde D. Is All MRI-SIJ Inflammation the Same? Gradient of Structural Damage with Increasing Cumulative Inflammation at the SIJ Quadrant Level in Axial Spondyloarthritis – 5-Year Data from the DESIR Cohort [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/is-all-mri-sij-inflammation-the-same-gradient-of-structural-damage-with-increasing-cumulative-inflammation-at-the-sij-quadrant-level-in-axial-spondyloarthritis-5-year-data-from-the-desir-co/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-all-mri-sij-inflammation-the-same-gradient-of-structural-damage-with-increasing-cumulative-inflammation-at-the-sij-quadrant-level-in-axial-spondyloarthritis-5-year-data-from-the-desir-co/