Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Use of ambulatory surgery in arthroplasty is increasing, but the need for transfusion mandates hospital admission. Despite the significant drop in transfusion rate linked to antifibrinolytic therapy, a significant number of patients are still transfused. Few prior studies have assessed primary rheumatologic diagnosis- such as rheumatoid arthritis- as a risk factor for the need for transfusion. The purpose of this study is to determine preoperative factors associated with receiving a blood transfusion after total knee arthroplasty (TKA) to optimally use ambulatory surgery, and to determine whether RA patients experience higher rates of transfusion.
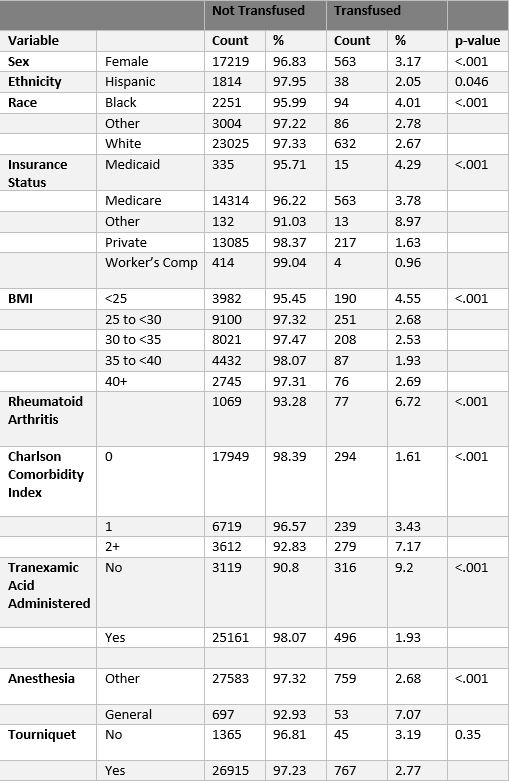
Methods: We retrospectively reviewed primary unilateral TKA patients from a single tertiary care institution from February 2016 to December 2022. Patient demographics, preoperative hemoglobin, BMI, diagnosis of RA, and tranexamic acid (TXA) use were obtained from the hospital electronic medical record. RA status was identified by ICD-10-CM diagnosis codes for RA or JIA (M05.x, M06.0x, M06.2x, M06.3x, M06.8x, M06.9x, M08.0x, M08.2x, M08.3x, M08.4x). The association of these variables with the primary outcome of receiving a packed red blood cell (RBC) transfusion was evaluated using the chi-square test or Fisher’s Exact Test, as appropriate, and in a multivariable logistic regression model.
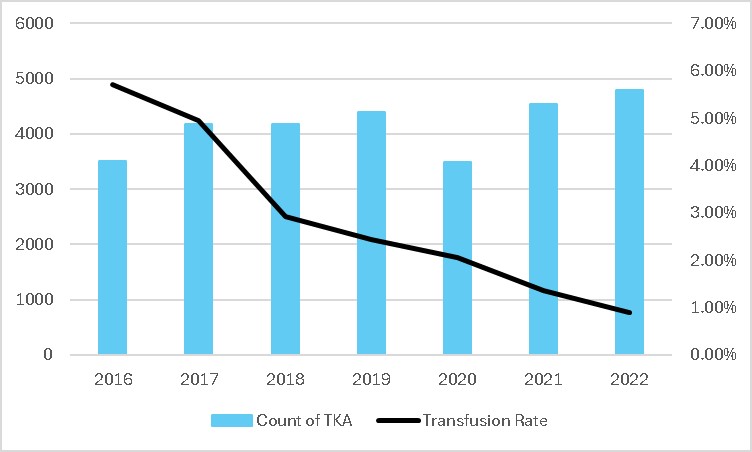
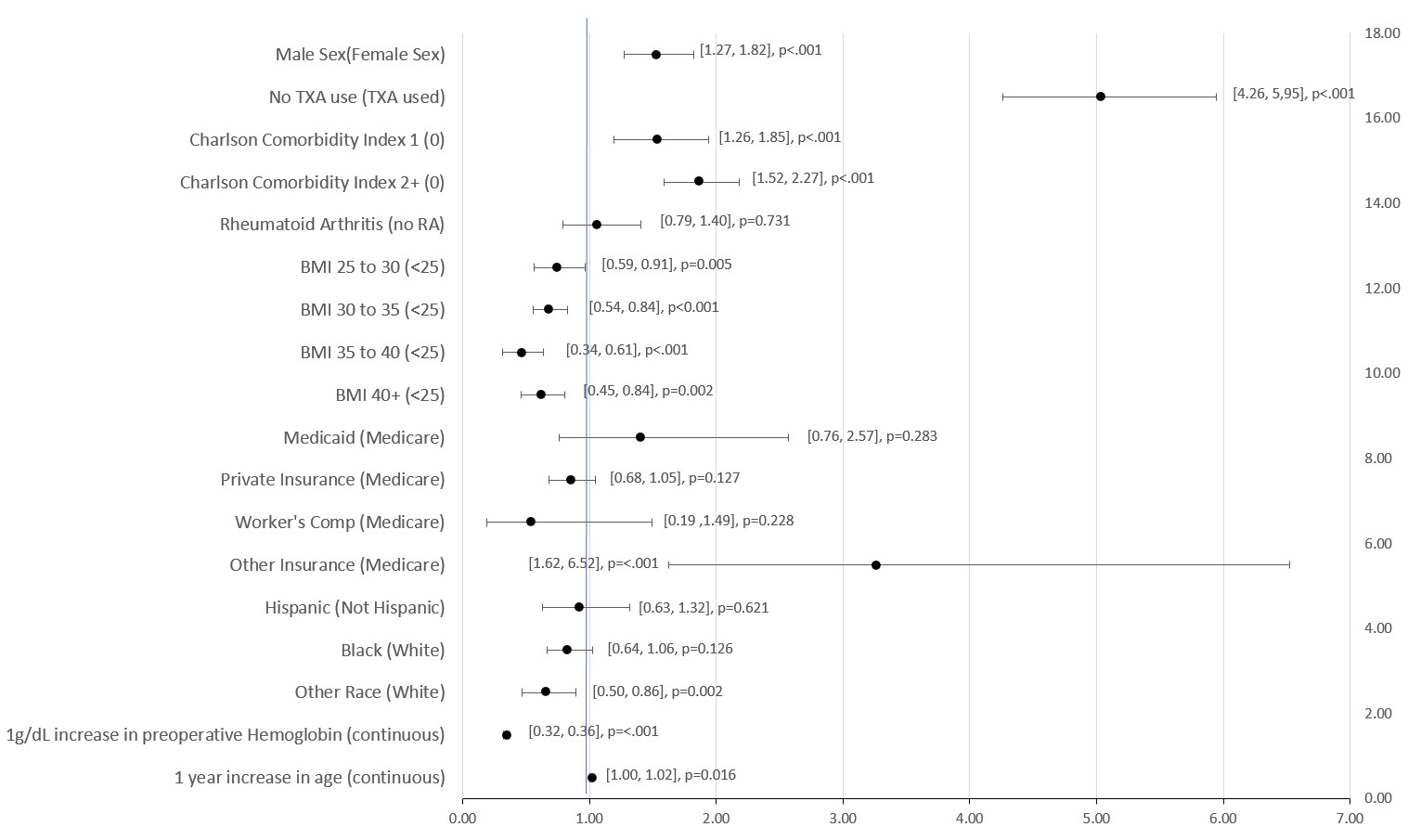
Results: There were 29,092 TKA included; 2.8% (822) received transfusions. Mean age was 67.1 years, mean preoperative hemoglobin was 13.5 g/dL, and 61.2% were female. 62.7% of patients had a Charlson Comorbidity score of 0 and 4.0% had a diagnosis of rheumatoid arthritis. Transfusion rate declined over the study period from 5.7% in 2016 to 0.9% in 2022. Risk factors for transfusion included male sex (odds ratio (OR) 1.52, 95% confidence interval (CI): 1.27, 1.82) and higher Charlson Comorbidity index (1 vs 0: OR 1.53, 95% CI: 1.26, 1.85 and 2+ vs 0: OR 1.86, 95% CI: 1.52, 2.27). Each 1 g/dL increase in preoperative hemoglobin decreased the risk of transfusion (OR 0.34, 95% CI: 0.32, 0.36). No TXA use increased the risk of transfusion (OR 5.03, 95% CI: 4.26, 5.95). Diagnosis of RA was not a significant risk factor for transfusion as compared to the general population. (OR 1.03, 95% CI: 0.79, 1.40).
Conclusion: Higher preoperative hemoglobin and use of TXA decreased the likelihood of having a transfusion, while male sex and higher comorbidity burden increased the risk of transfusion. RA was not a significant risk factor for transfusion. Significant preoperative factors should be assessed in patients being considered for ambulatory TKR to reduce the need for subsequent admission and transfusion. Future analysis should determine the optimal hemoglobin cut-off to avoid admission for transfusion.
To cite this abstract in AMA style:
Batter S, Do H, Sun D, Deeb A, Bui T, Blevins J, Figgie M, Lee G, Gibbons J, Mehta B, Goodman S, A Russell L. Investigating Predictors of Transfusion in Rheumatoid Arthritis and Osteoarthritis Patients Undergoing Knee Arthroplasty [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/investigating-predictors-of-transfusion-in-rheumatoid-arthritis-and-osteoarthritis-patients-undergoing-knee-arthroplasty/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigating-predictors-of-transfusion-in-rheumatoid-arthritis-and-osteoarthritis-patients-undergoing-knee-arthroplasty/