Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Sclerosis (SSc) patients often experience gastrointestinal complications, frequently managed with proton pump inhibitors (PPIs). Despite evidence of PPI-related chronic kidney disease (CKD) risk in the general population, its impact in scleroderma remains uncertain. This study aims to elucidate this association by comparing CKD incidence between PPI users and non-users. Utilizing the TrinetX database, a retrospective analysis was conducted to investigate this potential link. Findings from this analysis contribute valuable insights into optimizing therapeutic strategies and mitigating long-term renal complications in SSc patients.
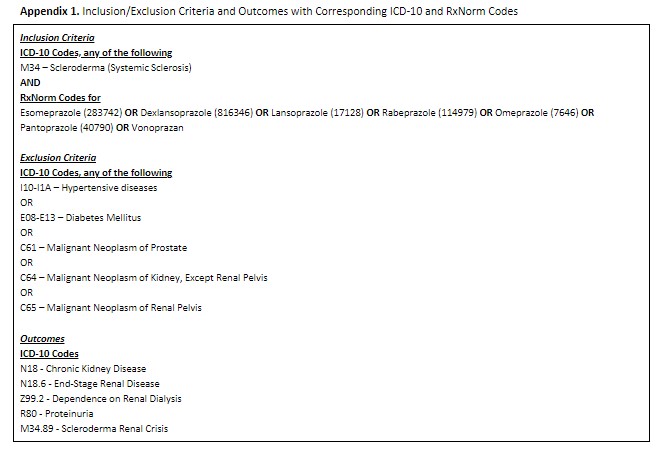
Methods: In this study, patients aged 18-99 were divided into two groups: those SSc who were on PPIs, regardless of dosing and those who were not. Inclusion criteria were standardized across both groups, requiring a diagnosis of SSc of any severity. Exclusion criteria included hypertensive diseases, diabetes mellitus, cystic kidney disease, prostate or renal cancer. Diagnoses were identified using ICD-10 codes, and RxNorm codes were used for medication identification (Appendix 1). Cohort comparability was ensured through 1:1 propensity score matching for age, gender, and ethnicity. The index event was defined as the appearance of SSc and PPIs in patient records. Primary outcomes included the diagnosis of CKD of any stage, End-Stage Renal Disease (ESRD), dependence on hemodialysis, proteinuria, and Scleroderma Renal Crisis. Patients with pre-existing conditions were excluded from the analysis, thus CKD was not used during matching.
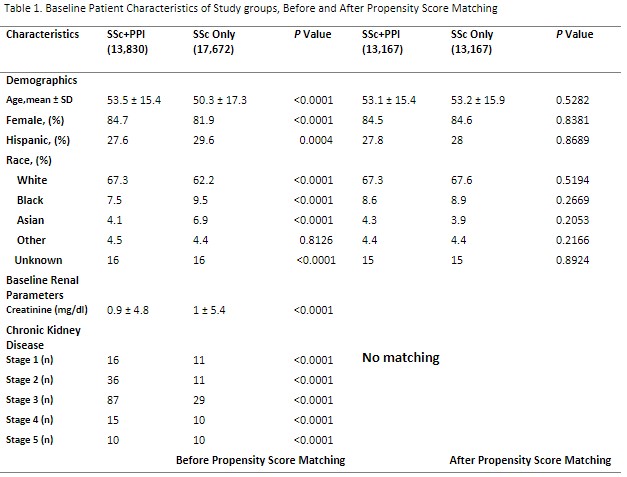
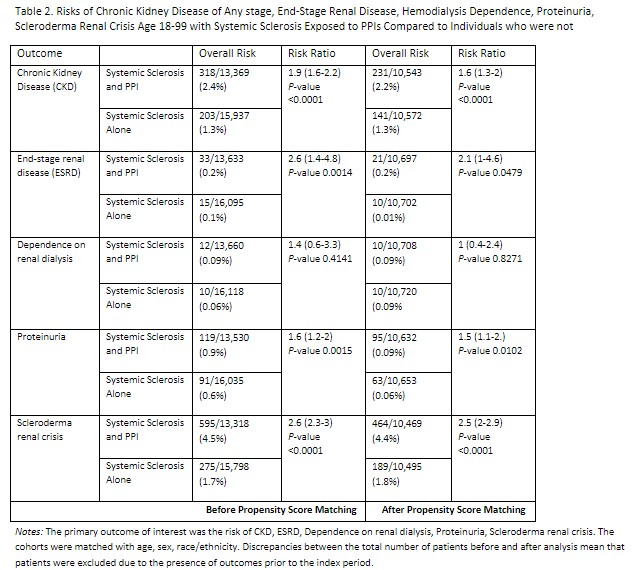
Results: With initial analysis there were 13,830 SSc patients on PPIs, whereas 17,672 had no PPI exposure. Both groups had more than 80% of females and were predominantly white. Cohorts demonstrated similar baseline creatinine and percentage of CKDs in their charts (Table 1). Before propensity score matching, PPI group demonstrated statistically significant higher risk of CKD (RR (Relative Risk) 1.9, 95% CI 1.6-2.2, p < 0.01), ESRD (RR 2.6, 95% CI 1.4-4.8, p 0.0014), proteinuria (RR 1.6, 95% CI 1.2-2, p 0.0015), Scleroderma renal crisis (RR 2.6, 95%CI 2.3-3, p < 0.01), while the risk of dialysis dependence was not significant. After matching, significant associations persisted for CKD, proteinuria, and Scleroderma Renal Crisis, but not for dialysis dependence or ESRD (Table 2).
Conclusion: This study unveils a noteworthy link between proton pump inhibitor (PPI) usage and increased risks of renal complications among Systemic Sclerosis (SSc) patients. Notably, the risk of Scleroderma Renal Crisis stands out as particularly pronounced. However, it’s essential to acknowledge limitations, including potential underreporting of symptoms in physician documentation, likely dose-dependent effects, and the concurrent use of other confounding agents. These findings accentuate the importance of exercising caution when prescribing PPIs to SSc patients and highlight the urgent need for further research to delve into the underlying mechanisms and refine therapeutic approaches accordingly.
To cite this abstract in AMA style:
Tskhakaia I, Lau A. Investigating Kidney Disease Risks in Systemic Sclerosis (SSc) – Effects of Proton Pump Inhibitors (PPI): Retrospective Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/investigating-kidney-disease-risks-in-systemic-sclerosis-ssc-effects-of-proton-pump-inhibitors-ppi-retrospective-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigating-kidney-disease-risks-in-systemic-sclerosis-ssc-effects-of-proton-pump-inhibitors-ppi-retrospective-analysis/