Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: It is unknown whether early changes in the menisci (e.g., intrameniscal signal alterations) have long-term consequences. We conducted a study to assess the prognostic potential of intrameniscal signal alterations with incident destabilizing meniscal tears (radial or complex tears or macerated menisci) or accelerated knee osteoarthritis (KOA).
Methods: We used existing magnetic resonance (MR)-based data from a sex-matched nested case-control study of 3 groups from the Osteoarthritis Initiative without radiographic KOA at baseline (Kellgren-Lawrence [KL] < 2): 1) accelerated KOA: developed KL 3 or 4 within 48 months; 2) typical KOA: increased in KL grade within 48 months (excluding accelerated KOA); 3) no KOA: no change in KL grade within 48 months. From the original groups (n = 375), we included people with intact medial and lateral menisci at baseline (n = 226) and 48-month meniscal data (n = 221). Two readers read annual intermediate-weighted MR sequences with and without fat-suppression from baseline to the 48-month visit using a modified version of the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine meniscal tear classification. The readers assessed 3 regions (anterior, body, posterior) of the medial and lateral menisci. Baseline meniscal status was operationally defined: 1) normal (intact with no signal intensity abnormalities) and 2) intrameniscal signal alteration (intrameniscal increased signal on a fluid-sensitive sequence that does not extend to an articular surface). We defined an incident destabilizing meniscal tear as the emergence of a radial (including root tears) or complex tear or maceration. Our readers had good inter-reader agreement (medial meniscal interobserver kappa = 0.90; lateral meniscal kappa = 0.63). We used 2 logistic regression models to assess 1) whether the presence of medial intrameniscal signal alteration (predictor) was associated with an incident medial destabilizing meniscal tear versus no incident medial destabilizing meniscal tear (reference group), and 2) if the presence of intrameniscal alterations in either meniscus predicted incident accelerated versus typical KOA (reference group) over the next 4 years.
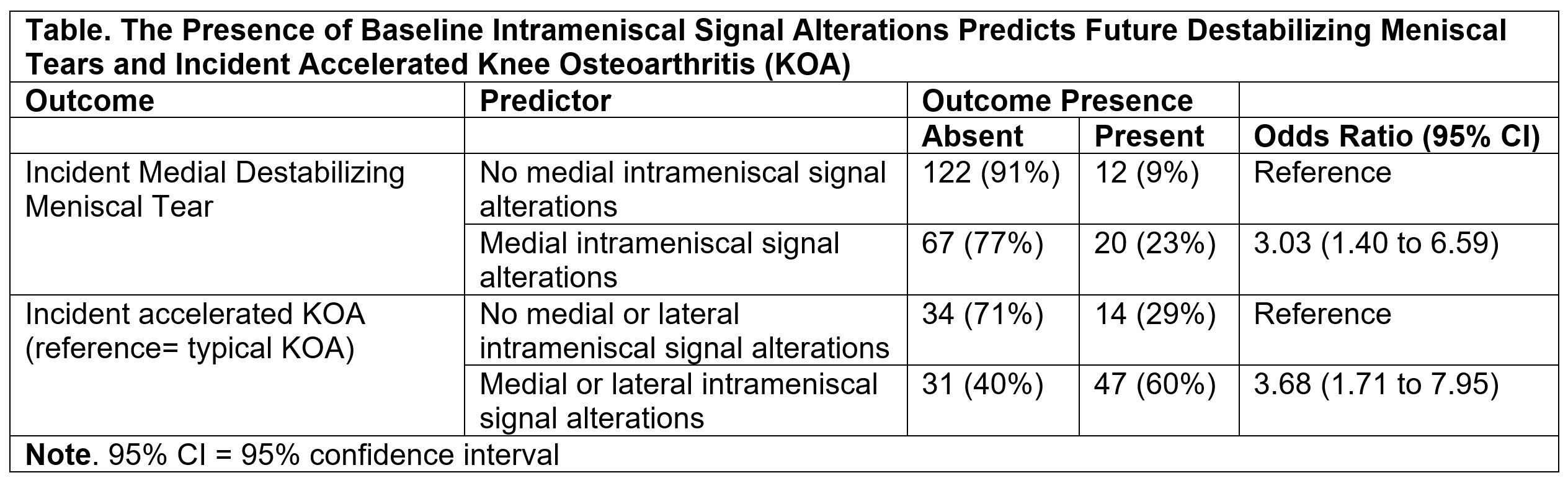
Results: We analyzed 221 knees with intact medial and lateral menisci at baseline. Overall, the study sample was mostly female (68%), with an average age of 58 (8) years, and an average body mass index of 28.1 (4.8) kg/m2. The presence of medial intrameniscal signal alterations was strongly associated with incident medial destabilizing meniscal tears (odds ratio = 3.0 [95% CI = 1.4 to 6.6]; Table). Though numbers were small, 8 out of 9 incident lateral destabilizing meniscal tears had lateral intrameniscal signal alterations at baseline. The presence of baseline intrameniscal signal alteration in a knee strongly predicted the onset of accelerated versus typical KOA (odds ratio = 3.7 [95% CI = 1.7 to 8.0]; Table).
Conclusion: Intrameniscal signal alterations on intermediate-weighted fat-suppressed images may be clinically meaningful as they relate to future outcomes. Intrameniscal signal alterations may be a potential therapeutic target and warrant further study.
To cite this abstract in AMA style:
Driban J, MacKay J, McAlindon T, Harkey M, Lu B, Eaton C, Lo G, Barbe M, Ward R. Intrameniscal Signal Alterations Strongly Predict Destabilizing Meniscal Tears and Accelerated Knee Osteoarthritis: Data from the Osteoarthritis Initiative [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/intrameniscal-signal-alterations-strongly-predict-destabilizing-meniscal-tears-and-accelerated-knee-osteoarthritis-data-from-the-osteoarthritis-initiative/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intrameniscal-signal-alterations-strongly-predict-destabilizing-meniscal-tears-and-accelerated-knee-osteoarthritis-data-from-the-osteoarthritis-initiative/