Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Dispersion is defined as the variability in an individual’s performance across multiple tasks at a single assessment visit. This measure has been studied in a number of neurodegenerative and neurodevelopmental disorders, in which increased dispersion was generally found to be associated with cognitive dysfunction (CD). We aim to compute a dispersion score using the tests of the American College of Rheumatology Neuropsychological battery (ACR-NB) and to determine the association between this dispersion score and the risk of CD in SLE patients.
Methods: This retrospective longitudinal study included patients who attended the Lupus Clinic from January 2016 to October 2019. A total of 301 adult SLE patients were administered the ACR-NB at their initial visit, 6 months and 12 months. CD was defined as a z-score of ≤-1.5 on ≥2 domains or z ≤-2 on ≥1 domain. The 19 tests of the ACR-NB were used to compute a type of dispersion score, the intraindividual standard deviation (ISD). To obtain the ISD, the standard deviation of the age- and sex- adjusted z-scores was calculated for each visit, resulting in a maximum of 3 scores per patient. To estimate the association between ISD and patient’s cognitive status (CD and non-CD), we used multi-level logistic regression, adjusting for clinically important covariates.
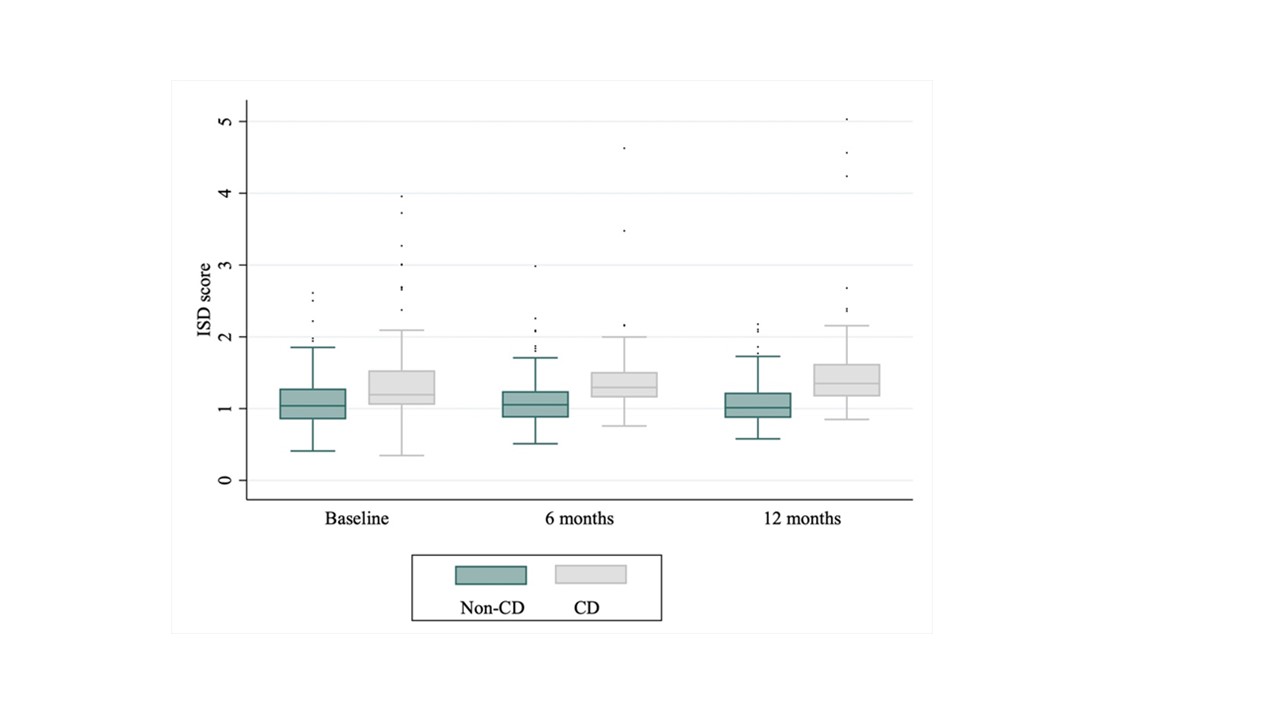
Results: CD was observed in 106 patients (35.2%) at baseline, 52 patients (27.8%) at 6 months, and 53 patients (28.0%) at 12 months. Among all observations across 3 visits, the mean age- and sex-adjusted ISD was 1.40 ± 0.55. Prior to adjustment for covariates, the mean ISD for the non-CD group was 1.10 ± 0.31 compared with 1.50 ± 0.70 for the CD group. After adjusting for ethnicity, education, employment, socioeconomic status and anxiety/depression, there was a statistically significant association between ISD and cognitive status (odds ratio [OR] for one unit increase in ISD: 13.56, 95% CI: 4.80-38.31; OR for 1/10th unit increase in ISD: 1.30, 95% CI: 1.17-1.44). Findings were robust to multiple sensitivity analyses. Multivariable random intercept logistic regression modelling is provided in Table 1. ISD scores across 3 assessment visits for non-CD and CD patients is provided in Figure 1.
Conclusion: Dispersion scores such as ISD have been explored as a pragmatic and sensitive marker of cognitive function in different patient populations. We showed that among adult SLE patients, increased ISD across the cognitive tests of the ACR-NB was associated with an increased likelihood of having CD, adjusting for important covariates. Additional research is warranted to evaluate the promise of dispersion scores in clinical practice.
To cite this abstract in AMA style:
He J, Diaz-Martinez J, Bingham K, Su J, Kakvan M, Tartaglia M, Ruttan L, Beaton D, Wither J, Choi M, Fritzler M, Anderson N, Bonilla D, Green R, Katz P, Touma Z. Insight into Intraindividual Variability Across Neuropsychological Tests and Its Association with Cognitive Dysfunction in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/insight-into-intraindividual-variability-across-neuropsychological-tests-and-its-association-with-cognitive-dysfunction-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/insight-into-intraindividual-variability-across-neuropsychological-tests-and-its-association-with-cognitive-dysfunction-in-patients-with-systemic-lupus-erythematosus/