Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Dermatomyositis (DM) and polymyositis (PM), collectively known as idiopathic inflammatory myositis (IIM), are autoimmune disorders characterized by inflammation of skeletal muscle, especially in the proximal group. Data on inpatient epidemiology, resource utilization, and healthcare expenditures of IIM are not well described. The aim of this study was to explore those characteristics using a large national inpatient database.
Methods: This retrospective cohort study used the data from the National Inpatient Sample (NIS), the largest public inpatient database in the US, in the year 2005-2014. Data for more than seven million individual hospitalization across all-payers from over 4,000 non-federal acute care hospitals across 40 states are recorded annually in the NIS database. All patients with ICD9-CM diagnostic codes for DM or PM were included. Patients with inclusion body myositis were excluded. The primary outcome was determining the inpatient prevalence of IIM. Secondary outcomes included determining inpatient mortality, morbidity, most common discharge diagnoses, resource utilization, hospital length of stay (LOS), and inflation-adjusted total hospital costs and charges. Multivariate regression analyses were used to adjust for age, gender, Charlson Comorbidity Index, income in patient zip code, hospital region, location, size, and teaching status.
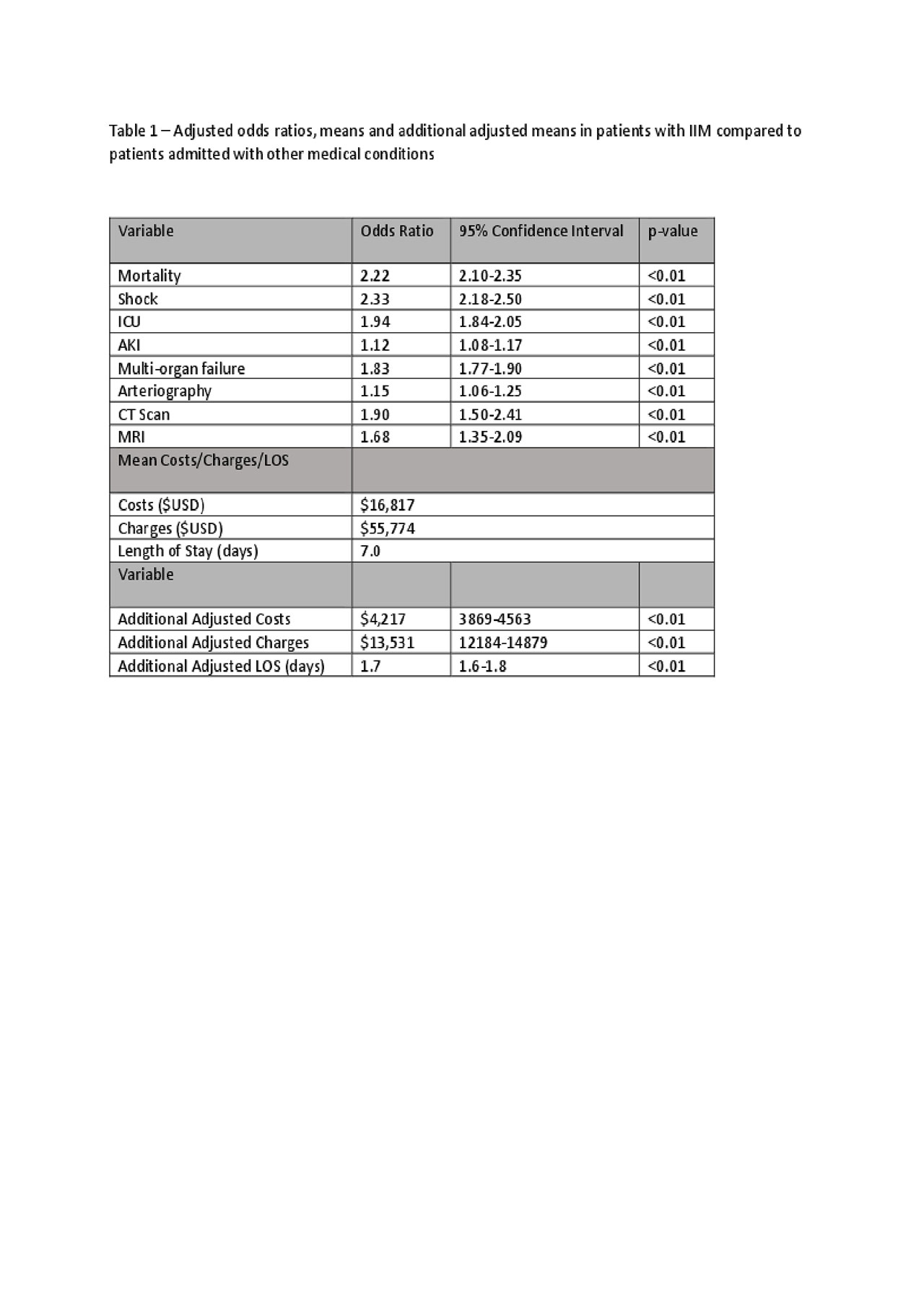
Results: A total of 160,528 admissions of patients with a diagnosis of DM/PM occurred in the study period. The mean age was 58.0 years and 68.7% were female. For the primary outcome, the inpatient prevalence of DM/PM was 41.9 cases per 100,000 discharges. The most common reasons for hospitalization were DM/PM itself, pneumonia, sepsis, AKI, and urinary tract infection. Patients with DM/PM displayed significantly increased odds of inpatient all-cause mortality compared to patients admitted for all other causes. Patients with DM/PM displayed significantly higher morbidity odds of shock, ICU stay, AKI, and multiorgan failure when compared to patients admitted for all other reasons. Patients with DM/PM were also found to have increased odds of utilizing special investigations, including CT, MRI, and arteriography. Patients with associated diagnosis of DM/PM displayed higher hospital costs, charges and LOS compared to patients with no DM/PM (Table 1).
Conclusion: The inpatient prevalence of DM/PM was higher than what would be expected from the overall incidence. Hospitalizations of these patients were associated with a significantly higher morbidity and mortality. The mean total hospital costs, charges, and LOS for patients admitted with DM/PM were higher than patients without DM/PM.
To cite this abstract in AMA style:
Ungprasert P, Cheungpasitporn W, Thongprayoon C, Wijarnpreecha K, Kroner P. Inpatient Epidemiology of Dermatomyositis and Polymyositis in the United States [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/inpatient-epidemiology-of-dermatomyositis-and-polymyositis-in-the-united-states/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inpatient-epidemiology-of-dermatomyositis-and-polymyositis-in-the-united-states/