Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Due to the rarity of polyarteritis nodosa (PAN), no study has ever investigated inpatient characteristics, healthcare utilization and frequency of comorbidities of patients with PAN. The current study was conducted with the aim to better describe those information using data from a large national database.
Methods: Patients with PAN were identified from the Nationwide Inpatient Sample (NIS) database for the year 2014 using ICD-9 diagnostic codes. The primary outcome was determining the inpatient prevalence of PAN in hospitalized patients in the US. Secondary outcomes included determining inpatient mortality, morbidity, comorbidities, hospital length of stay (LOS) and expenditures. Expenditures were sub-divided into total hospitalization charges and hospital costs. Total hospital charges represent the amount of money that each hospital billed the payers for the service provided during each admission, while hospital costs represent the amount of money the hospital invested to provide care during each admission. A cohort of patients without PAN was also identified from the same database to serve as comparators for analysis of comorbidities. Multivariate regression analysis was used to adjust for age, sex, ethnicity and hospital characteristics.
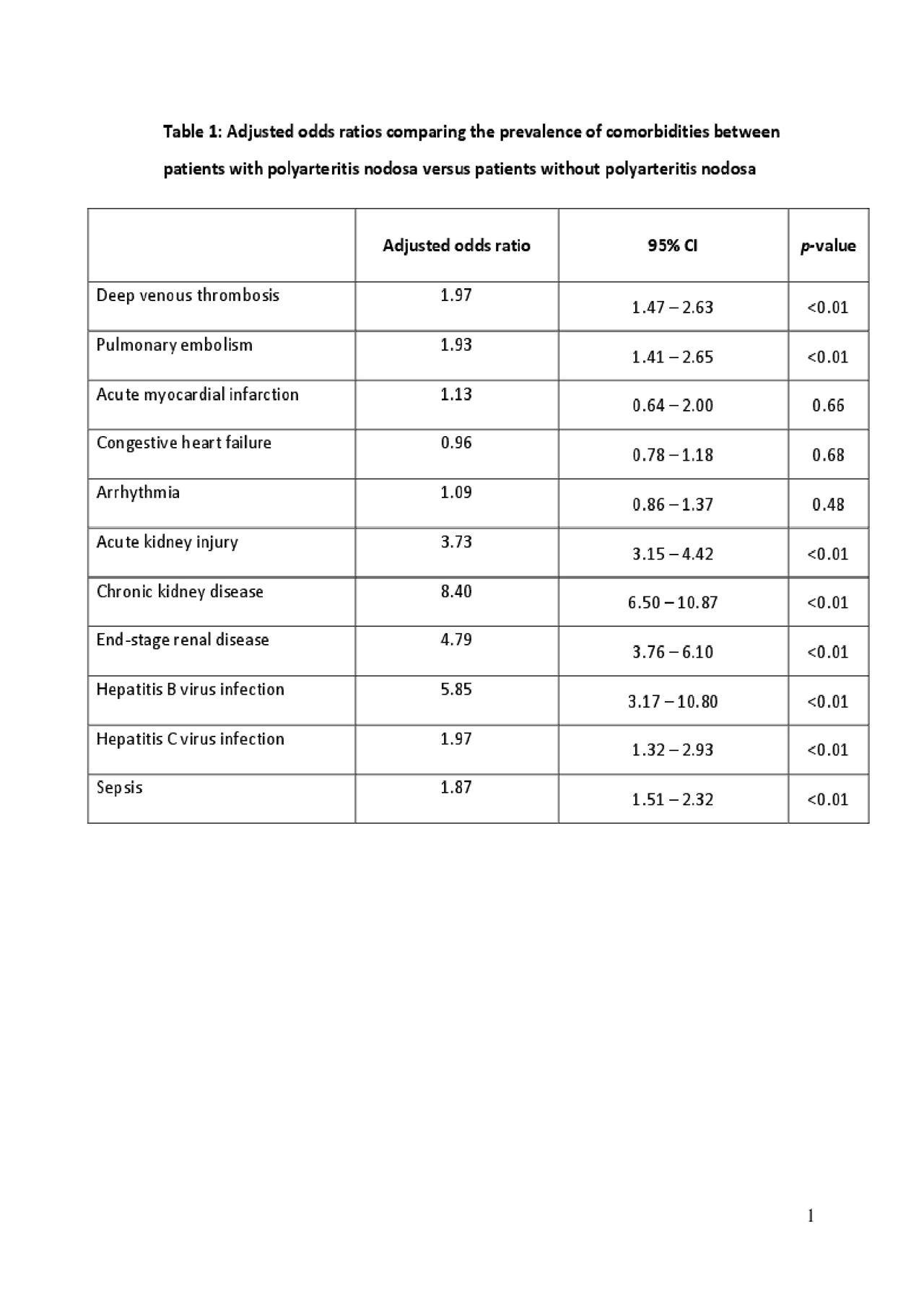
Results: A total of 4,110 patients with PAN were included in the study. The mean age was 59.5 years and 61% were female. The inpatient prevalence of PAN was 11.6 cases per 100,000 admissions. The most common reasons for admission among patients with PAN in this database were as follows; PAN itself (17.6%), sepsis (6.9%), acute kidney injury (4.9%), acute respiratory failure (2.1%) and pneumonia (2.0%). During hospitalization, a significantly higher morbidity among patients with PAN was observed as indicated by a significantly higher risk of shock (adjusted OR 1.75; 95% CI, 1.23 – 2.50), admission to ICU (adjusted OR 1.88; 95% CI, 1.44 – 2.45) and multi-organ failure (adjusted OR 3.12; 95% CI, 2.64 – 3.69) although the odds of mortality was not significantly elevated (adjusted OR 1.35; 95% CI, 0.91 – 2.00). Patients with PAN also displayed significantly higher hospital costs (additional adjusted mean [aAM]: $9,693, p< 0.01), hospitalization charges (aAM: $34,273, p< 0.01) and LOS (aAM: 4.1 days, p< 0.01) compared to patients without PAN. Analysis of comorbidities found a significant association between PAN and several comorbidities as shown in table 1.
Conclusion: The inpatient prevalence of PAN is higher than what would be expected from the overall general prevalence. Hospitalizations of patients with PAN are associated with significantly higher rates of morbidity and expenditures.
To cite this abstract in AMA style:
Ungprasert P, Koster M, Cheungpasitporn W, Wijarnpreecha K, Thongprayoon C, Kroner P. Inpatient Burden, Expenditures and Comorbidities of Polyarteritis Nodosa: National Inpatient Sample 2014 [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/inpatient-burden-expenditures-and-comorbidities-of-polyarteritis-nodosa-national-inpatient-sample-2014/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inpatient-burden-expenditures-and-comorbidities-of-polyarteritis-nodosa-national-inpatient-sample-2014/