Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Palliative medicine prioritizes quality of life and relief of suffering in serious illness. Despite high morbidity and mortality in rheumatic disease, data suggests that palliative care (PC) remains underutilized. In this study, we sought to analyze the current inpatient and outpatient referral practices to PC for patients with rheumatic disease at a single academic institution.
Methods: A medical records extraction tool was used to identify eligible patients for retrospective chart review. First, all patients seen at our institution’s outpatient rheumatology clinics over the preceding 5 years were filtered by referral to ambulatory PC from rheumatology clinic. Next, all patients seen by the inpatient rheumatology consult team over the preceding 1 year were filtered by co-consultation of inpatient PC. Inpatients were excluded if the reason for rheumatology consultation ended up not being for a true rheumatic reason. Chart review was performed on these patients to identify demographics, rheumatic diagnosis, prior Advance Care Planning (ACP), reason for referral, outcome of referral, and cause of death if applicable. For inpatient consults, factors also included reason for inpatient rheumatology consultation and if rheumatology-initiated PC consultation. Data analysis was performed using descriptive statistics.
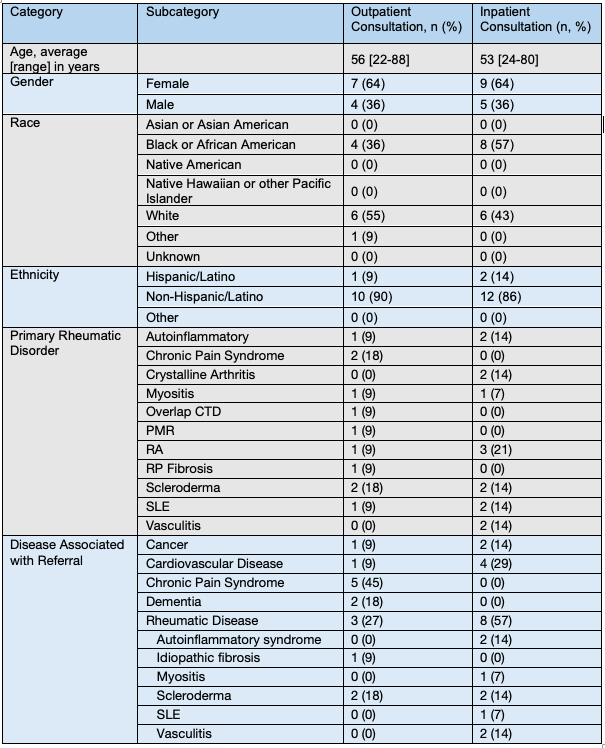
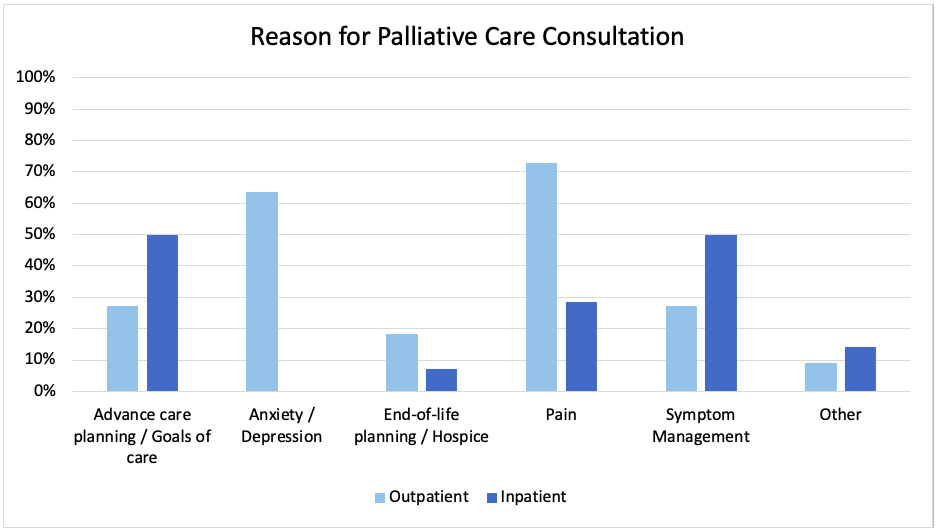
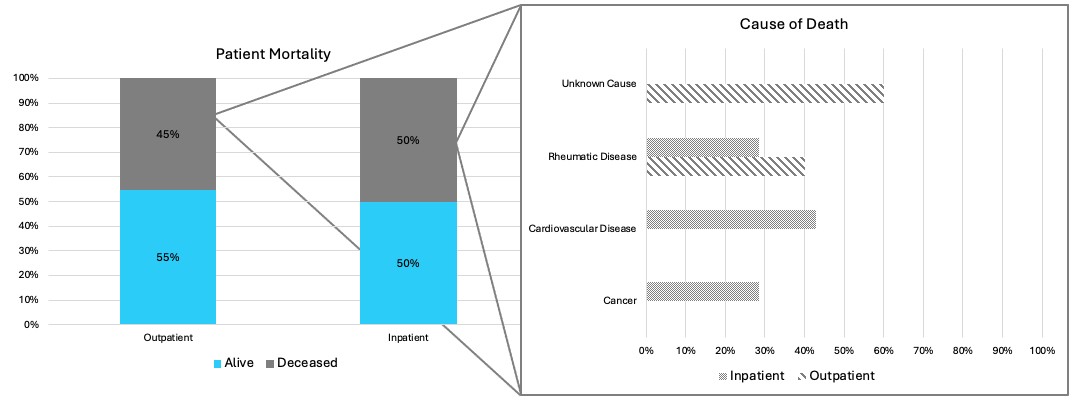
Results: Of the 18,441 patients seen in rheumatology clinics over the preceding 5 years, 11 (0.06%) were referred to ambulatory PC. Of the 527 inpatients seen by rheumatology over the preceding 1 year, 29 (6%) were also seen by inpatient PC consultants. 15 were excluded, resulting in 14 out of 527 (3%) inpatients. Patient characteristics are shown in Table 1. Of inpatients, most had a prior rheumatic diagnosis at time of consult (n=12, 86%). Reasons for consultation are shown in Figure 1. Only 1 outpatient (9%) and 1 inpatient (7%) had prior ACP before seeing PC. Rarely was inpatient PC referral initiated by rheumatology (n=2, 14%). Nearly half of outpatients (n=5, 45%) were deceased by the time of chart review; average time of death following referral was 190 days [76-478] (Figure 2). No inpatients died during hospitalization and 7 (50%) were deceased at the time of chart review; average time of death following hospitalization was 139 days [1-332].
Conclusion: Data from our academic institution demonstrates that patients with rheumatic disease are rarely referred to PC and rates of ACP are low. When PC referral does occur, mortality for these patients is high, perhaps due to late timing of referral. Patients seen by PC have a wide spectrum of age and underlying rheumatic diagnosis. Similarly, the reason for PC involvement varies among patients. Rheumatic disease contributes substantially to mortality when death occurs. Further research is needed to better define the need for earlier and more frequent identification of patients appropriate for referral to PC.
To cite this abstract in AMA style:
Herndon S, Kimball J, Leverenz D. Inpatient and Outpatient Palliative Care Referral Practices for Patients with Rheumatic Disease: Retrospective Chart Review at a Single Academic Medical Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/inpatient-and-outpatient-palliative-care-referral-practices-for-patients-with-rheumatic-disease-retrospective-chart-review-at-a-single-academic-medical-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inpatient-and-outpatient-palliative-care-referral-practices-for-patients-with-rheumatic-disease-retrospective-chart-review-at-a-single-academic-medical-center/