Session Information
Date: Tuesday, November 15, 2016
Title: Muscle Biology, Myositis and Myopathies - Poster II: Clinical
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Polymyositis (PM)/dermatomyositis (DM) is a chronic inflammatory disorder that affects muscle, skin and lung in various degree, and interstitial lung disease (ILD) is a major cause of death. In clinical setting, it is necessary to predict future clinical manifestations and outcomes accurately before initiation of treatment. In this study, we examined initial predictors of poor survival in patients with PM/DM-associated ILD.
Methods: This study used a database of a multicenter retrospective cohort of Japanese patients with PM/DM-associated ILD (JAMI cohort), which involved 44 institutions across Japan. Inclusion criteria of the JAMI cohort were adult-onset, definite or probable PM/DM including clinically amyopathic DM (CADM), ILD confirmed by imaging study, and availability of sera at diagnosis. Demographic features, diagnosis, clinical features, laboratory findings, high-resolution CT patterns and treatment regimens used were retrospectively collected. Serum samples were subjected to autoantibody assays; enzyme-linked immunosorbent assay for anti-melanoma differentiation-associated gene 5 (MDA5) and RNA immunoprecipitation for anti-aminoacyl–tRNA synthetase (ARS). Cumulative survival rates were calculated using the Kaplan-Meier method and equality of survival curves was tested by the Breslow test. The best model for predicting survival was searched using multivariate analysis using step-wise selection of parameters and the Cox proportional hazards regression model.
Results: This study enrolled 497 patients, including 76 (15%) with PM, 158 (32%) with classic DM, 263 (53%) with CADM (median observation period: 20 months, IQR 5-43). Autoantibody analysis revealed 209 (42%) positive for anti-MDA5 and 166 (34%) positive for anti-ARS antibodies. By univariate analysis, age at onset (>60 years), male, CADM, fever, Raynaud phenomenon, absence of muscle weakness, skin ulceration, CRP (>1 mg/dL), CK (<750 IU/L), aldolase (<17.5 IU/L), SP-D (<100 ng/mL), ferritin (>500 ng/mL), random GGA pattern on CT, SpO2 (<95%), positive anti-MDA5, and negative anti-ARS were identified as initial parameters associated with subsequent mortality. By testing various combinations of parameters selected by univariate analysis, we propose a model consisting of independent predictors of poor survival rates (Figure). In terms of treatment regimens introduced, use of calcineurin inhibitors was associated with better survival rates while corticosteroid pulse therapy and intravenous immunoglobulin were associated with poor outcomes.
Conclusion: Using a large cohort of well-defined patient population, we have successfully identified independent predictors of short-term mortality in patients with PM/DM-associated ILD.
Figure: Multivariate analysis for predictors of poor prognosis: Estimated hazard ratios for mortality with the 95% confidence intervals 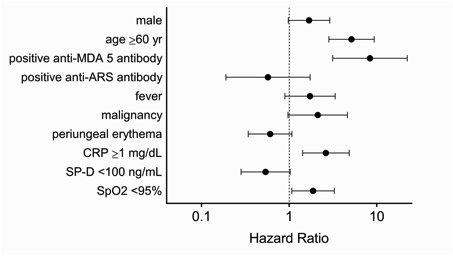
To cite this abstract in AMA style:
Sato S, Masui K, Nishina N, Kawaguchi Y, Kawakami A, Tamura M, Ikeda K, Nunokawa T, Tanino Y, Asakawa K, Kaneko Y, Gono T, Kuwana M. Initial Predictors of Short-Term Poor Survival Rates in Patients with Polymyositis/Dermatomyositis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/initial-predictors-of-short-term-poor-survival-rates-in-patients-with-polymyositisdermatomyositis-associated-interstitial-lung-disease/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/initial-predictors-of-short-term-poor-survival-rates-in-patients-with-polymyositisdermatomyositis-associated-interstitial-lung-disease/
