Session Information
Session Type: Abstract Session
Session Time: 1:30PM-1:45PM
Background/Purpose: Women with systemic rheumatic diseases (SRDs), and particularly those on immunosuppressive medications, are at increased risk for serious infections such as influenza and COVID-19. While current guidelines recommend vaccination with non-live vaccines for patients with SRDs, patient uptake of vaccines in real-world settings remain unclear.
Methods: Women aged 18-65 evaluated at least twice by a rheumatologist at the Hospital for Special Surgery (HSS) who were enrolled in the HSS Rheumatology Women’s Reproductive Health and Wellness Cohort between 2022-2024 were included. All subjects had an SRD diagnosis by ICD-10 code-based algorithms and completed demographic, medical history, and vaccination questionnaires. Bivariate analyses compared demographic, socioeconomic, lifestyle, and clinical factors of patients ever versus never vaccinated for influenza or COVID-19. Multivariable models evaluated factors associated with ever versus never vaccination for COVID-19 and influenza vaccination separately.
Results: Of 740 participants (mean age 47.4±12.4 years, 538 [72.7%] White, 98 [13.2%] Hispanic or LatinX, 668 (84.6%) self-reported ever receiving influenza vaccination and 719 (97.2%) reported receiving COVID-19 vaccination. Compared to unvaccinated patients, women vaccinated for influenza more frequently had a Bachelor’s degree or higher (88.0% vs 75.0%), were married/partnered (67.1% vs 48.6%), on immunosuppressive medications (60.2% vs 47.9%), saw a primary care physician (PCP) (78.0% vs 56.9%) or gynecologist (75.5% vs 54.2%) at least yearly, and had an inflammatory arthritis (IA) diagnosis (62.2% vs 44.1%), but were less frequently on corticosteroids (12.0% vs 20.8%). Participants ever vs. never vaccinated for COVID-19 were more frequently married/partnered (66.0% vs 42.9%), privately insured (88.4% vs 70.0%), employed (71.1% vs 38.1%), ever used alcohol (83.8% vs 61.9%), and saw a PCP (76.6% vs. 52.4%) or gynecologist (74.0% vs 52.4%) at least yearly, but were less frequently on corticosteroids (12.2% vs 33.3%) [Table 1, p< 0.05]. Among patients never vaccinated for influenza, participants with IA versus connective tissue diseases were more likely to cite vaccine side effects as a reason for not getting vaccinated (19.2% vs 0.0%). In multivariable analyses, the odds of never receiving influenza vaccination were greater among individuals with < 1 PCP visit per year (OR 2.78, 95% CI [1.52–5.06]), but lower among those taking immunosuppressive medications (OR 0.45, 95%CI [0.24–0.84]) [Table 2]. For COVID-19, the odds of never receiving vaccination were greater among those who were Black versus White (OR 4.15, 95% CI [1.04-14.3]) [Table 3].
Conclusion: Influenza and COVID-19 vaccination uptake was overall high in this cohort of women with SRDs, with notable associations between black race, immunosuppressive medication use, and frequency of PCP visits with vaccination status. Factors associated with COVID-19 vaccination should be interpreted cautiously due to few unvaccinated women in the current study. Addressing concerns about side effects and improving access to routine care may further optimize vaccination uptake.
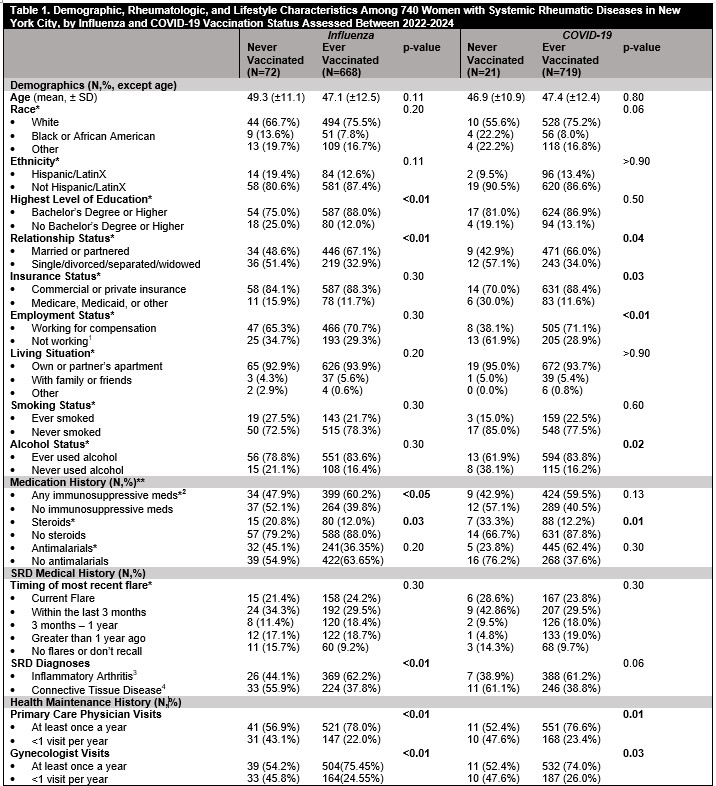 P-value < 0.05=statistically significant. *Column values within each category may not add up due to individuals who preferred not to answer the specific question. **Current medication use at the time of data collection. 1. Includes individuals with disability, retired, unemployed, and students; 2. Includes Abatacept, Adalimumab, Anakinra, Anifrolumab, Belimumab, Canakinumab, Certolizumab, Denosumab, Etanercept, Golimumab, Guselkumab, Infliximab, Ixekizumab, Mepolizumab, Rilonacept, Risakizumab, Rituximab, Sarilumab, Secukinumab, Tocilizumab, Ustekinumab, Azathioprine, Cyclophosphamide, cyclosporine, leflunomide, methotrexate, mycophenolate, sulfasalazine, tacrolimus, thalidomide, voclosporin, baricitinib, tofacitinib, upadicitinib; 3. Includes Ankylosing spondylitis, JRA, PSA, Spondyloarthritis, Enteropathic arthritis, PMR, Polyarthritis; 4. Includes APS, SLE, Overlap CTDs, UCTD, Myositis, Systemic Sclerosis, Eosinophilic fasciitis.
P-value < 0.05=statistically significant. *Column values within each category may not add up due to individuals who preferred not to answer the specific question. **Current medication use at the time of data collection. 1. Includes individuals with disability, retired, unemployed, and students; 2. Includes Abatacept, Adalimumab, Anakinra, Anifrolumab, Belimumab, Canakinumab, Certolizumab, Denosumab, Etanercept, Golimumab, Guselkumab, Infliximab, Ixekizumab, Mepolizumab, Rilonacept, Risakizumab, Rituximab, Sarilumab, Secukinumab, Tocilizumab, Ustekinumab, Azathioprine, Cyclophosphamide, cyclosporine, leflunomide, methotrexate, mycophenolate, sulfasalazine, tacrolimus, thalidomide, voclosporin, baricitinib, tofacitinib, upadicitinib; 3. Includes Ankylosing spondylitis, JRA, PSA, Spondyloarthritis, Enteropathic arthritis, PMR, Polyarthritis; 4. Includes APS, SLE, Overlap CTDs, UCTD, Myositis, Systemic Sclerosis, Eosinophilic fasciitis.
.jpg) A p-value of < 0.05 was considered statistically significant. Patients who chose not to respond were excluded from the model.
A p-value of < 0.05 was considered statistically significant. Patients who chose not to respond were excluded from the model.
.jpg) A p-value of < 0.05 was considered statistically significant. Patients who chose not to respond were excluded from the model.
A p-value of < 0.05 was considered statistically significant. Patients who chose not to respond were excluded from the model.
To cite this abstract in AMA style:
Kim Y, Kannayiram S, Smole A, Masto L, Nagpal N, Piatchou Donfack N, Jannat-Khah D, Mandl L, Siegel C, Lieber S, Lockshin M, Sammaritano L, Barbhaiya M. Influenza and COVID-19 Vaccination Uptake Among Women with Systemic Rheumatic Diseases in New York City Assessed Between 2022 and 2024 [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/influenza-and-covid-19-vaccination-uptake-among-women-with-systemic-rheumatic-diseases-in-new-york-city-assessed-between-2022-and-2024/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/influenza-and-covid-19-vaccination-uptake-among-women-with-systemic-rheumatic-diseases-in-new-york-city-assessed-between-2022-and-2024/
