Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Women with SLE have an elevated risk of cardiovascular disease. Many women with SLE frequently report chest pain in the absence of obstructive coronary artery disease (CAD) due to coronary microvascular dysfunction (CMD), a form of ischemia with no obstructive CAD (Manchanda et al, 2022). Echocardiographic studies have shown that SLE patients have reduced left ventricular (LV) function, which may also correlate with higher SLE disease activity scores (Gegenava et al, 2020). As such, we used cardiac magnetic resonance imaging (cMRI) to investigate the relationship between SLE, related inflammatory biomarkers, and cardiac function in female SLE patients.
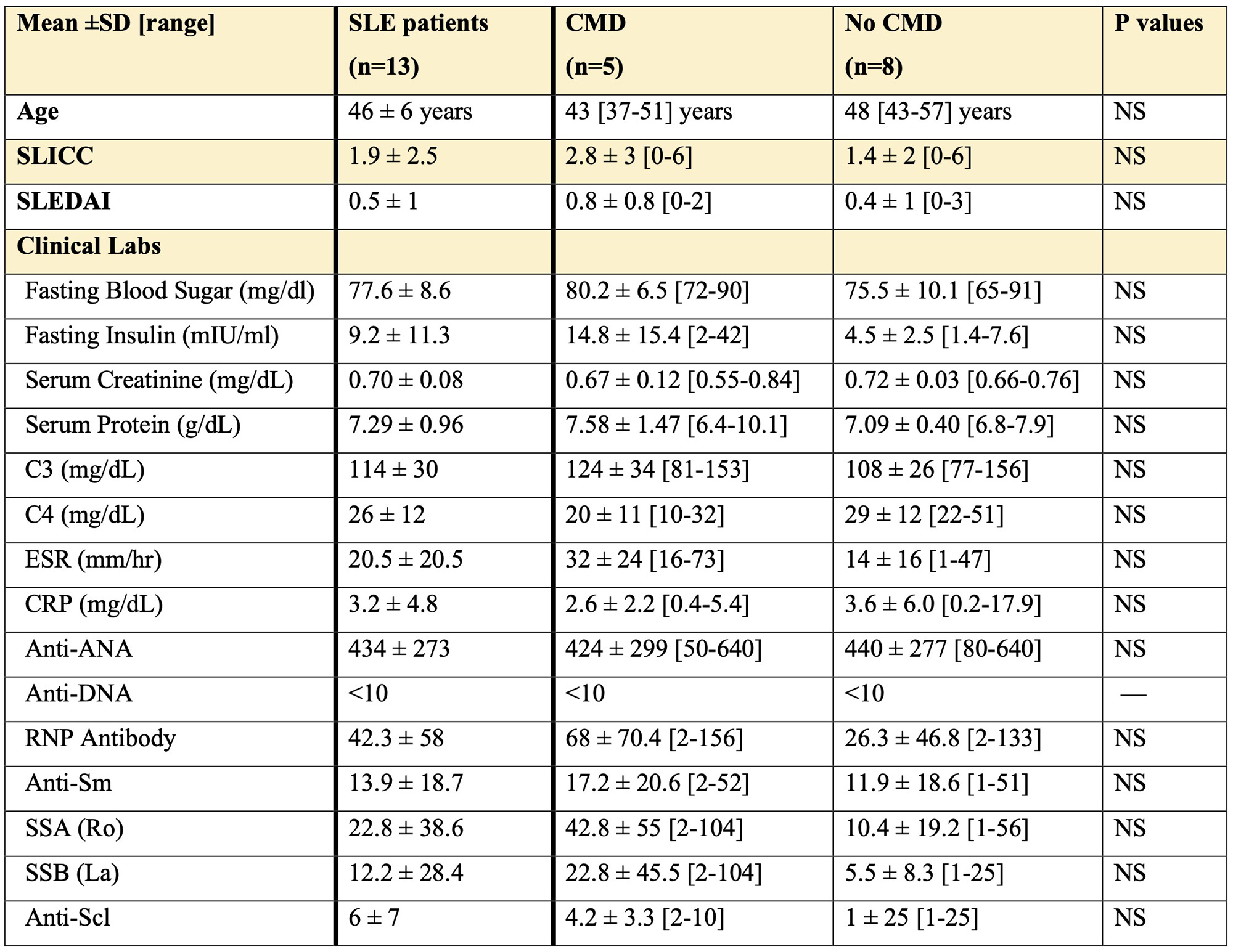
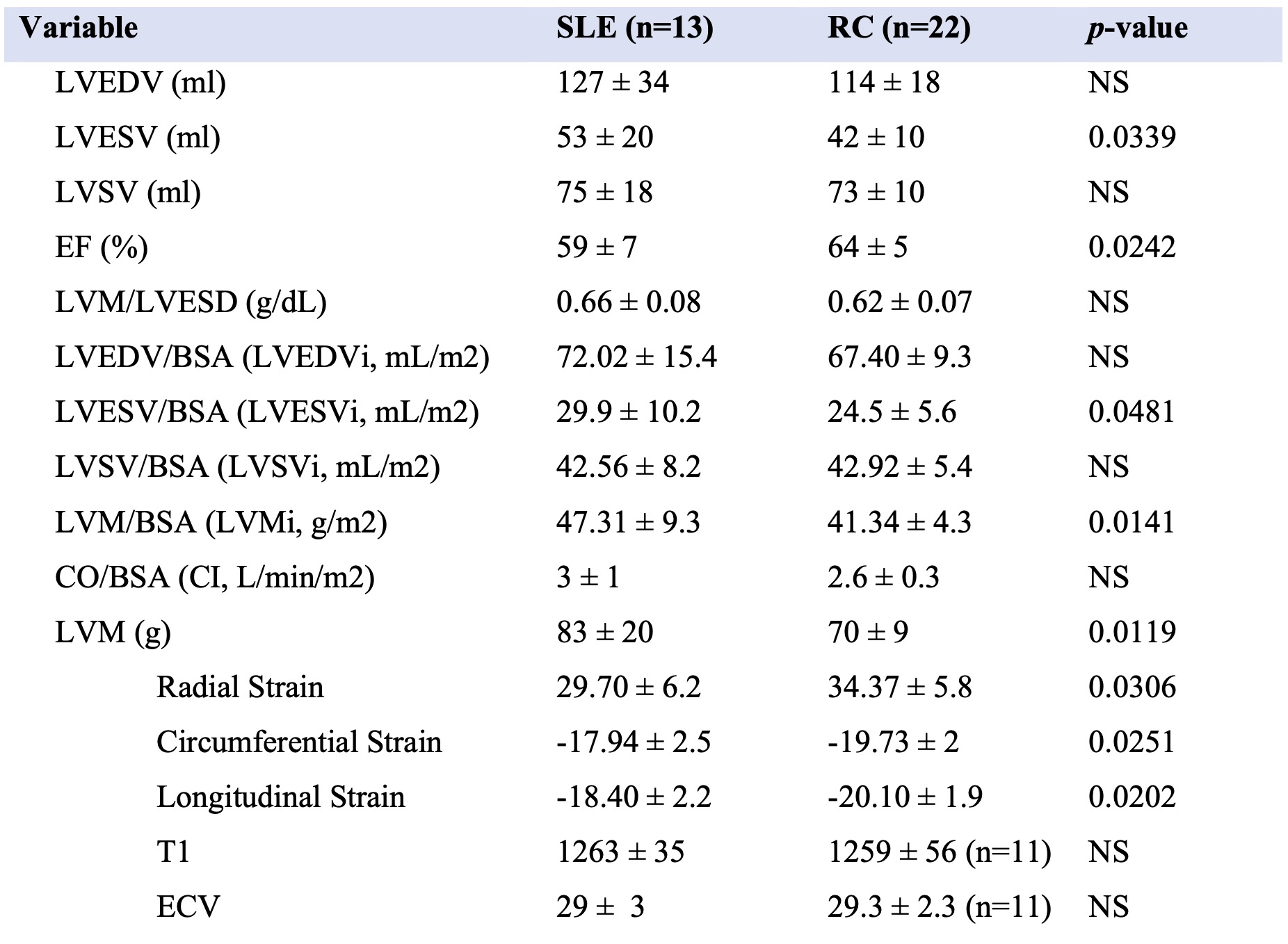
Methods: We performed stress cMRI in women with SLE and chest pain with no obstructive CAD (n=13, all met ACR 1997 criteria, Table 1) and reference controls (n=22) using our published protocol (Aldiwani et al, 2022). We evaluated LV function, tissue characterization (T1 mapping, ECV), and delayed enhancement, using CV142 software (Circle Cardiovascular Imaging Inc, Calgary, AB, Canada). Myocardial perfusion reserve index (MPRI) was calculated using our published protocol (Thomson et al, 2015). SLEDAI and SLICC Damage Index (DI) were calculated per validated criteria (Bombardier et al, 1992, Gladman et al, 1997). Serum samples were analyzed for inflammatory markers and autoantibodies (Table 1). Independent two-tailed t test was performed on clinical values with CMD and no CMD SLE subjects, and on cMRI values with all SLE subjects and controls. Correlation analysis was done on clinical values, and cMRI values on all SLE subjects.
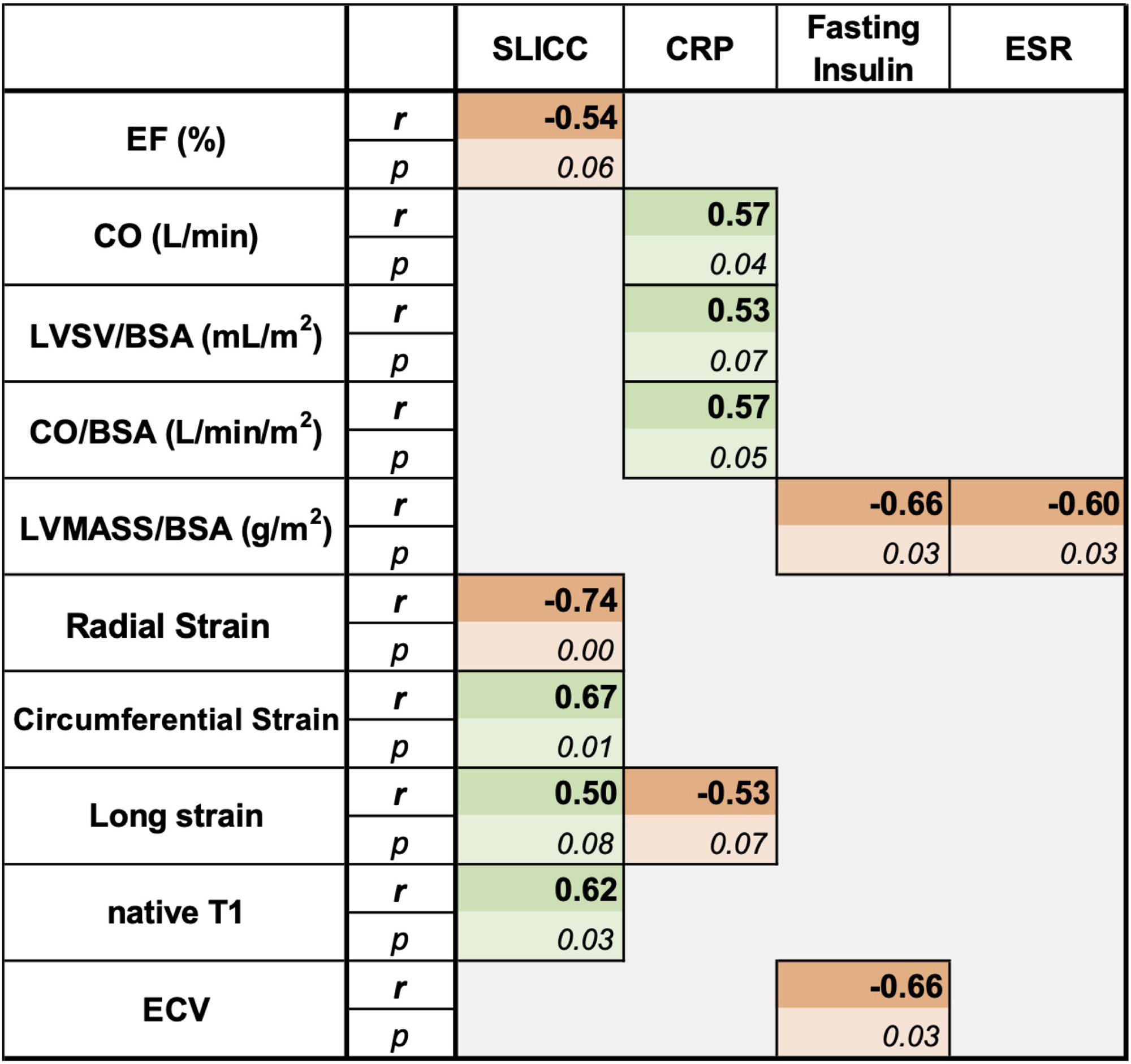
Results: Overall, 40% of SLE subjects had MPRI values < 1.84, consistent with CMD. Compared to controls, SLE subjects had significantly lower LVEF, and higher LVESVi and LVMi (Table 2). Corresponding to this, radial, longitudinal, and circumferential strain were significantly lower in the SLE subjects. In correlation analysis of serum inflammatory biomarkers to cMRI values in the SLE subjects, SLICC DI was related to worse cardiac function (lower radial, circumferential and longitudinal strain) and higher T1 time (Table 3). Additionally, fasting insulin and ESR were negatively correlated with LVMi. Fasting insulin also negatively correlated with ECV. CRP had a positive association with LVESV index and CI and a negative association with longitudinal strain.
Conclusion: Among women with SLE with chest pain and no obstructive CAD, 40% have CMD. While evaluations of known inflammatory markers (such as ESR and CRP) predictably correlated with decreased cardiac function (Lertratanakul et al, 2014), our study found that decreased fasting insulin levels is a novel marker associated with diminished LV function. In addition, although studies have used SLEDAI as a marker of disease activity when assessing cardiac dysfunction, we are the first to demonstrate that SLICC DI, an assessment of SLE damage, is also correlated with cardiac dysfunction in SLE. This indicates that SLE patients with higher SLICC DI and increased SLE-related damage could potentially have silent involvement in their cardiac tissue, and as such, SLICC DI is another tool that can be used to evaluate the association between SLE and LV dysfunction.
To cite this abstract in AMA style:
Hagiwara A, Bose M, Bernardo M, Nelson M, Ishimori M, Berman D, Bairey Merz C, wei j, Jefferies C. Inflammatory Markers and Left Ventricular Dysfunction in Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/inflammatory-markers-and-left-ventricular-dysfunction-in-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammatory-markers-and-left-ventricular-dysfunction-in-systemic-lupus-erythematosus-sle/