Session Information
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) and ankylosing spondylitis (AS) belong to a group of inflammatory arthritides known to share similar extra-articular manifestations, such as inflammatory bowel disease (IBD). Though, IBD, PsA, and AS individually present significant economic burden, it is not clear whether there is an incremental economic burden associated with IBD among patients with PsA or AS. This study aims to describe the prevalence and incidence of IBD and quantify the healthcare resource utilization (HRU) and direct healthcare costs associated with IBD among patients with PsA and AS.
Methods: Adult patients with ≥2 claims for PsA or AS were selected from a large US claims database (Q12007–Q32016). Prevalence and incidence of IBD, including Crohn’s disease (CD), ulcerative colitis (UC), and IBD-related gastrointestinal (GI) disturbances (gastroenteritis/colitis/gastritis) were assessed during the 1-year period following the initial claim for PsA/AS (i.e., study period) in PsA patients and AS patients separately. Prevalence and incidence for each individual condition were also reported. HRU and costs (2017 US$) were assessed during this period and compared between patients with (cases) and without (controls) IBD. Cases and controls were required not to have any IBD diagnosis during the 1-year period before their first claim for PsA/AS and were matched 1:1 on age, sex, region of residence, health plan type, index year, and employment status. The comparison of HRU and costs were conducted using Wilcoxon signed-rank test.
Results: We identified 22,205 PsA and 9,980 AS patients. IBD prevalence was 3.8% (CD: 1.0%; UC: 0.9%; GI disturbances: 2.5%) in PsA patients and 8.5% (3.8%; 2.7%; 4.2%) in AS patients. IBD incidence was 2.5% (0.4%; 0.3%; 2.0%) in PsA and 4.1% (1.0%; 0.8%; 2.9%) in AS. There were 464 PsA and 314 AS patients with IBD who were matched 1:1 with PsA and AS patients without IBD during the study period.
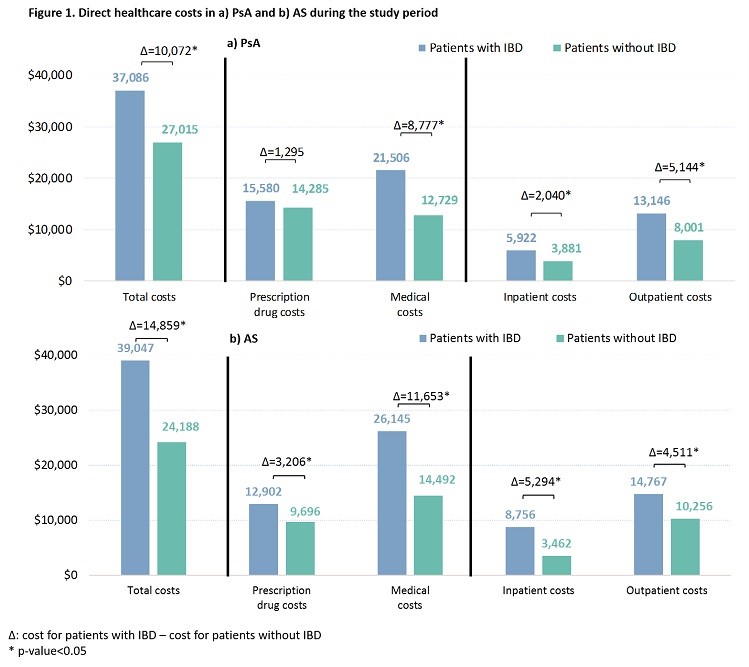
Patients with IBD had significantly higher HRU, including more outpatient (OP), emergency room, and inpatient (IP) visits, more IBD-related procedures (e.g., gastro-related endoscopy, abdominal/bowel imaging), and more corticosteroid use. In PsA, the mean annual total costs were $37,086 for patients with IBD, 27% higher than for patients without IBD (p<0.001; Figure 1); in AS, the costs were $39,047 for patients with IBD, 38% higher than for patients without IBD (p<0.001). The difference in total costs was largely driven by the difference in medical costs (PsA: 87%; AS: 78%). Of the medical cost difference, 23% and 59% were accounted for by the differences in IP and OP costs, respectively, in PsA patients, while the percentages were 45% and 39% in AS patients.
Conclusion: IBD prevalence and incidence were 3.8% and 2.5% in PsA and 8.5% and 4.1% in AS, respectively. In both PsA and AS, IBD was associated with substantial economic burden, including higher HRU and healthcare costs.
To cite this abstract in AMA style:
Bergman MJ, Zueger P, Song J, Pivneva I, Betts KA, Joshi AD. Inflammatory Bowel Disease Is Associated with a Substantial Economic Burden in Patients with Psoriatic Arthritis and in Patients with Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/inflammatory-bowel-disease-is-associated-with-a-substantial-economic-burden-in-patients-with-psoriatic-arthritis-and-in-patients-with-ankylosing-spondylitis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammatory-bowel-disease-is-associated-with-a-substantial-economic-burden-in-patients-with-psoriatic-arthritis-and-in-patients-with-ankylosing-spondylitis/