Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: There is evidence that in almost all patients with longstanding and active ankylosing spondylitis (AS) inflammatory lesions in the posterior elements are as frequent as in the anterior spine1. Therefore, it was argued that assessment of posterior structures should be embedded in routine diagnostic MRI assessment of the spine in patients with established AS or suspected of having AS1. However, little is known about the prevalence of lesions in the posterior elements in patients with recent onset axial spondyloartritis (axSpA). We investigated the prevalence of inflammatory lesions in the posterior elements in patients with and without inflammation in the vertebral bodies in patients with recent onset axSpA and patients with possible axSpA.
Methods: Patients with back pain (≥3 months, ≤2 years, onset <45 years) visiting the rheumatology outpatient clinics of the five participating centers were included in the SPondyloArthritis Caught Early (SPACE)-cohort (n=345). During the diagnostic work-up, all patients underwent MRI of the spine (MRI-spine). MRIs-spine were scored by 3 independent readers according to the ASAS consensus definition2 and the Canada-Denmark score3,4, including assessment of posterior elements1. The ASAS consensus definition states that evidence of anterior/posterior spondylitis in ≥3 sites is highly suggestive of axSpA. Therefore, we used a cut-off of ≥3 inflammatory lesions to mark an MRI-spine positive. Definite lesions were considered present if 2/3 readers agreed on it.
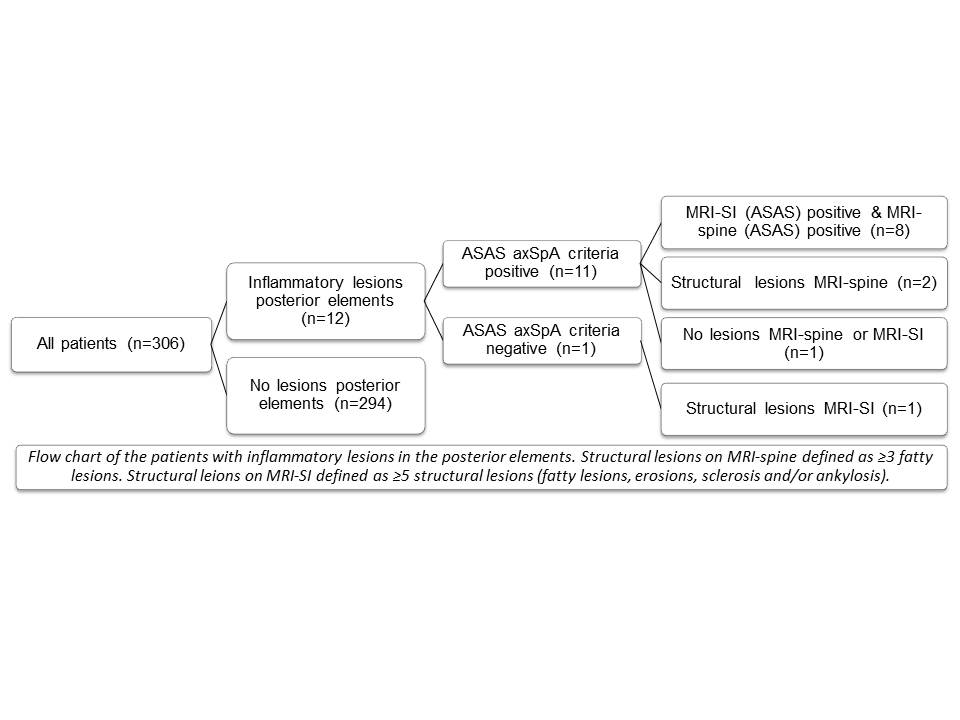
Results: Only patients with complete MRI-spine data were included in this analysis (n=306), of which 126 patients fulfilled the ASAS axSpA criteria5. In total, only 12/306 patients (3.9%) had inflammatory lesions in the posterior elements; 8 of them (66.7%) fulfilled the ASAS axSpA criteria (imaging-arm) and had also a positive MRI-spine. The remaining 4 patients (33.3%) had lesions in the posterior elements but no inflammatory lesions in the vertebral bodies, yet two out of four had signs of structural lesions (≥3 fatty lesions). Three out of these four patients fulfilled the ASAS axSpA criteria via the clinical-arm. The remaining patient had signs of structural lesions in the SI-joints (MRI) plus 3 other SpA-features (inflammatory back pain, good response to NSAIDs and elevated CRP and ESR) and has a clinical diagnosis of SpA by the rheumatologist.
Conclusion: The prevalence of inflammatory lesions in the posterior elements in the SPACE-cohort is low, suggesting that assessment of inflammatory lesions in the posterior elements in addition to the vertebral bodies gives only limited extra information in patients with recent onset axSpA and possible axSpA.
References: 1Maksymowych W. AC&R 2010;62:4-10. 2Hermann KG. ARD 2012;71:1278-88. 3Lambert R. J Rheumatol 2009;36 Suppl 84:3-17. 4Østergaard M. J Rheumatol 2009;36 Suppl 84:18-34. 5Rudwaleit M. ARD 2009;68:1520-7
Disclosure:
R. van den Berg,
None;
M. de Hooge,
None;
M. Reijnierse,
None;
V. Navarro-Compán,
None;
K. Fagerli,
None;
M. Turina,
None;
M. van Oosterhout,
None;
R. Ramonda,
None;
F. van Gaalen,
None;
T. Huizinga,
None;
D. van der Heijde,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammation-in-the-posterior-elements-of-the-spine-is-infrequent-in-patients-with-recent-onset-axial-spondyloarthritis-especially-if-no-inflammation-in-the-vertebral-bodies-is-observed/