Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) has a ‘pre-RA’ period that can be defined by elevations in autoantibodies to citrullinated protein antigens (ACPA) and rheumatoid factor (RF) prior to clinically-apparent inflammatory arthritis. ACPA and RF elevations can be used to predict future RA; however, most models of prediction have only used autoantibody data from a single time point. To address this gap, we evaluated changing autoantibody positivity and timing of future RA in a sample set of pre- and post-RA samples from the Department of Defense Serum Repository.
Methods: We evaluated serial pre- and post-RA diagnosis serum samples from a cohort of 215 individuals with RA (213 with RA classified by 1987 criteria; 2 cases by diagnosis by a board-certified rheumatologist). All samples were tested for ACPA using the CCP3 assay (Inova, positivity based on manufacturer’s recommendation) and RF-IgM, IgA and IgG (Inova, positivity based on level present in < 2% of healthy controls) We stratified cases by sex and utilized a Cox regression model that assumed a Markov renewal process to estimate the hazard of developing RA based on concurrent positivity of autoantibodies within individuals over time.
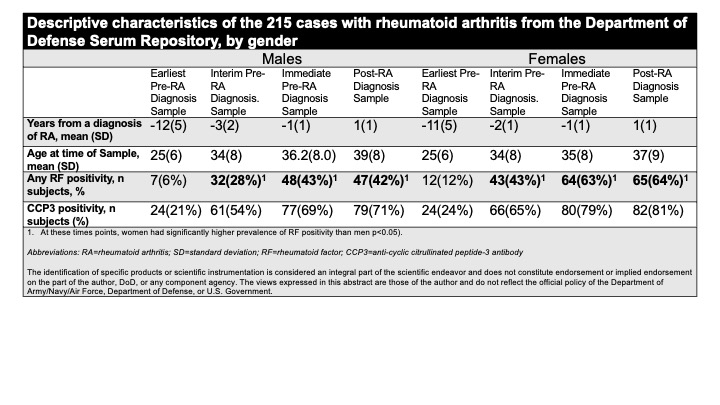
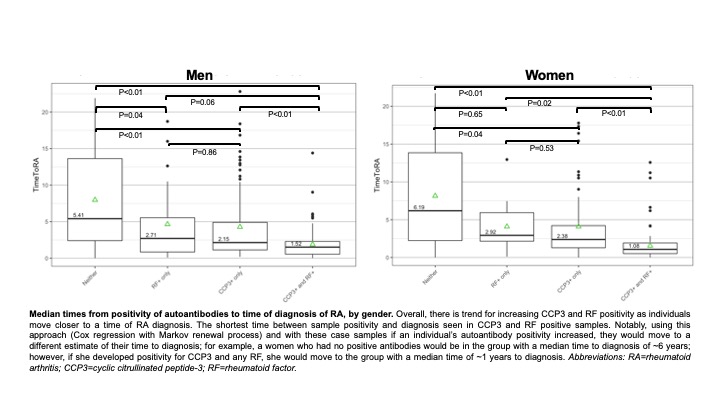
Results: Descriptive characteristics of the cases are presented in the Table. Overall, women were more likely than men to be positive for any RF pre- and post-RA diagnosis. Within cases stratified by gender, an increasing number of positive autoantibodies was associated with a shorter time to diagnosis of RA (Figure). In particular, positivity for CCP3 and any RF indicated a median time-to-diagnosis of RA of 1.52 years in men, and 1.08 years in women. Notably, if an individual’s autoantibody positivity increased, their hazard of developing RA would increase (i.e. their time to diagnosis would update to a new estimate) (Figure).
Conclusion: In this pre-RA cohort, prevalence of positivity of a combination of CCP3 and RF occur closer to diagnosis. This suggests an expansion of autoimmunity across the development of RA where biologic processes influencing both ACPA and RF production culminate in the transition to clinically-apparent RA. Furthermore, while predictive ability herein is limited given the retrospective design of this project, prior work has established that autoantibody positivity, especially ACPA positivity, is predictive for future RA (reviewed in Deane Arthritis Rheum 2021). As such, if these findings are further validated, they could be applied in a 2-step fashion to identify an individual’s overall risk for future RA, then evaluate the changing positivity of autoantibodies over time to estimate their evolving risk and timing of future RA. Notably, the literature regarding the rate of autoantibody positivity in RA in men and women is conflicting, and issues such as diagnostic bias can influence these findings; however, the gender differences seen herein in the prevalence of autoantibody positivity and prediction of timing of future RA needs further investigation. Finally, while additional study is needed, these findings also suggest that in clinical trials for RA prevention altering the development of new autoantibodies may be a measure to understand success of an intervention.
To cite this abstract in AMA style:
Bergstedt D, Peterson R, Feser M, Moss L, Thiele G, Mikuls T, Edison J, Holers V, Deane K. Increasing Rates of Positivity of Autoantibodies Indicates a Shorter Time-to-Diagnosis of Future Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/increasing-rates-of-positivity-of-autoantibodies-indicates-a-shorter-time-to-diagnosis-of-future-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increasing-rates-of-positivity-of-autoantibodies-indicates-a-shorter-time-to-diagnosis-of-future-rheumatoid-arthritis/