Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Cutaneous Lupus Erythematosus (CLE) is a chronic autoimmune skin disease characterized by a spectrum of cutaneous manifestations resulting from immune dysregulation and inflammation. While CLE is considered an organ-specific disease, its symptoms can manifest in the context of Systemic Lupus Erythematosus (SLE), alongside further systemic involvements. Portraying heterogeneity in dermatological findings, CLE is assessed and subclassified as Acute LE (ACLE), Subacute LE (SCLE) and Chronic or Discoid LE (CCLE, DLE) subject to rashes appearing as erythematosus, papular or butterfly shaped. Environmental factors and UV irradiation trigger the development of skin lesions, yet the origin of the disease is still undetermined. Lupus-specific autoantibodies are proven to be highly accurate diagnostic tools, as they offer insight into phenotypic variation.
Type I Interferons (IFNs) are antiviral cytokines associated with autoimmunity. IFNs trigger a signalling cascade leading to the induction of interferon-stimulated genes (ISGs). Increased ISG expression has been linked with SLE and typically indicates high disease activity. ISGs appeared overexpressed in the periphery and on skin tissues, where IFNκ was also upregulated in keratinocytes.
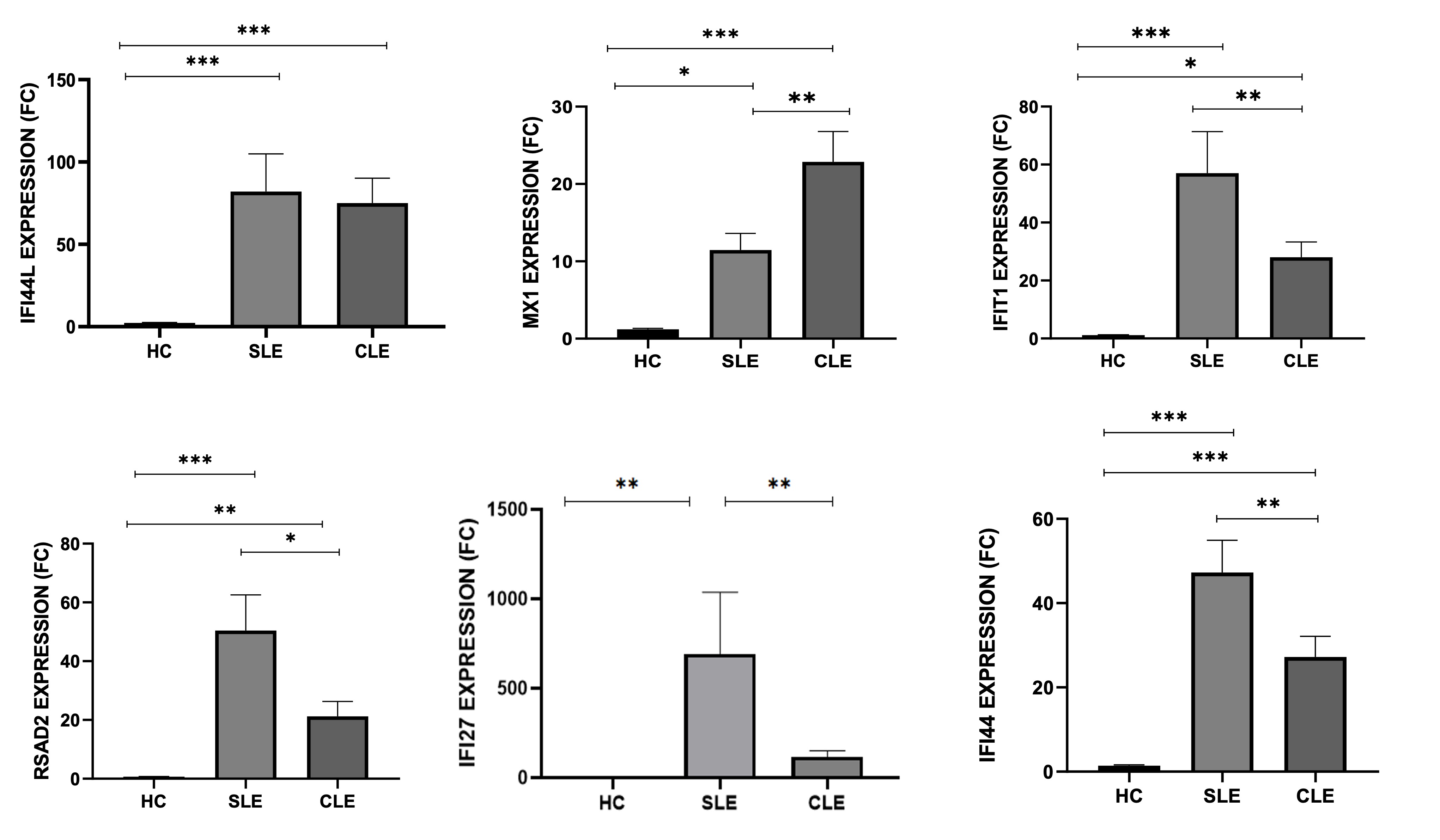
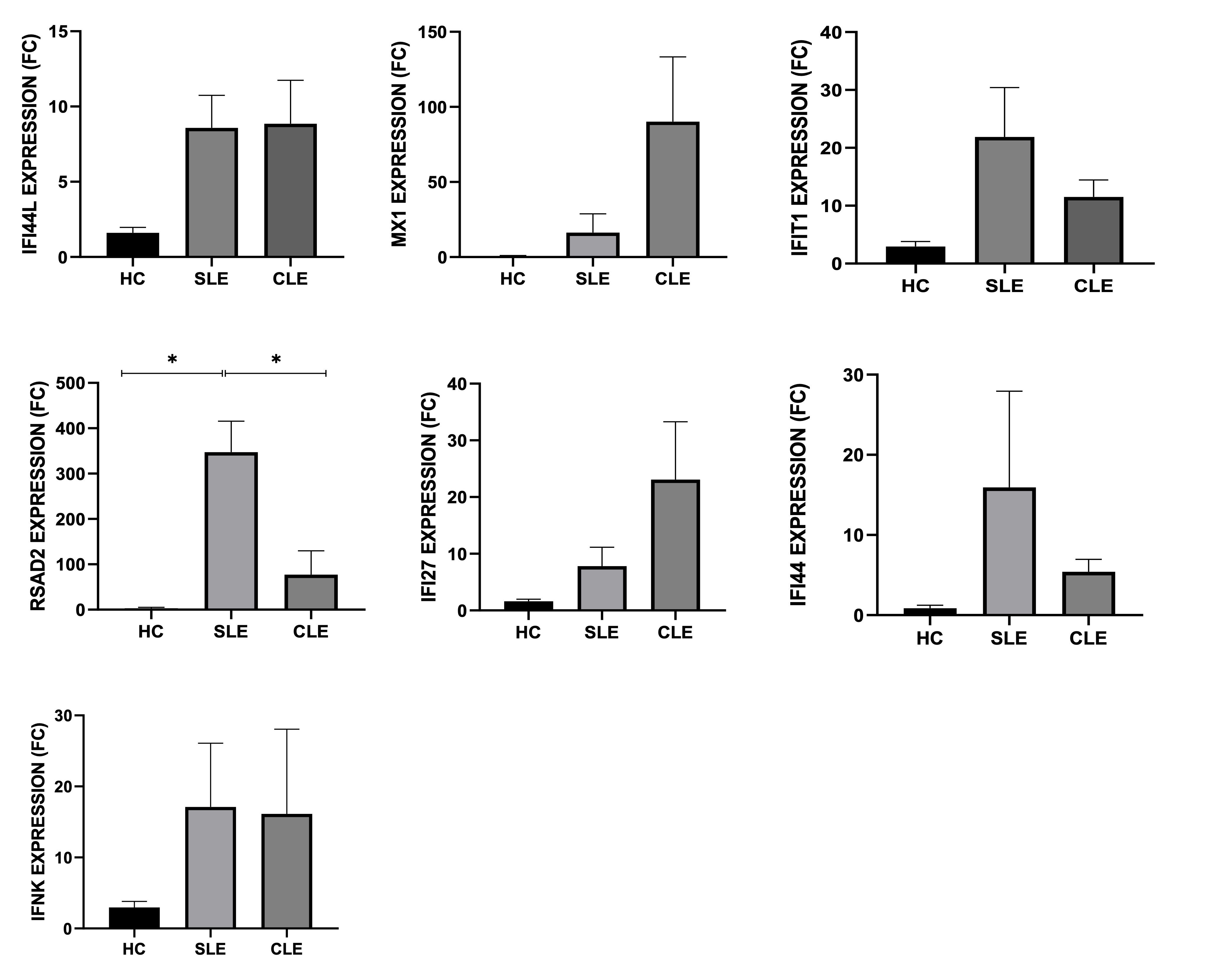
This study aimed to investigate the expression of Type I ISGs (MX1, IFIT1, RSAD2, IFIT27, IFI44, IFI44L) in the peripheral blood and skin biopsies of patients presented with cutaneous lesions compared to patients with systemic disease.
Methods: 65 whole peripheral blood samples and 30 skin biopsies from patients with Cutaneous lesions from SLE and CLE, stored in the Biobank of Molecular Physiology and Clinical Applications Unit, Department of Physiology, were acquired prior to treatment in collaboration with “Andreas Sygros” hospital, following clinical data evaluation. RNA isolation from both peripheral blood and homogenized biopsy tissues was used to synthesize cDNA for the quantification of the following Type I Interferon inducible genes: MX1, IFIT1, RSAD2, IFIT27, IFI44, IFI44L as well as IFNκ solely for biopsies, through qPCR. Patients fulfilled the ACR classification criteria and signed a written consent form before entering the cohort.
Results: SLE and CLE patients had increased expression of Type I ISGs in their peripheral blood, when compared to HCs. Specifically, CLE patients displayed IFI44L (p=0.0002), IFI44 (p< 0.0001), MX1 (p< 0.0001), IFI27 (p=0.0008), RSAD2 (p=0.0402) and IFIT1 (p=0.0053) expression versus HCs. Respectively, SLE patients had significantly higher IFI44L (p=0.0009), IFI44 (p< 0.0001), MX1 (p=0.0190), IFI27 (p< 0.0001), RSAD2 (p< 0.0001) and IFIT1 (p< 0.0001) expression compared to HCs. Gene expression between CLE and SLE patients showed significance in RSAD2 (p=0.0065), IFI27 (p=0.0008) and IFI44 (p=0.0099) expression with predominant gene upregulation in SLE patients. In skin biopsies however, gene expression was not significant between CLE and SLE patients.
Conclusion: In conclusion, alongside high ISG expression in SLE, our study validates high IFN signature in CLE, primarily in the peripheral blood where IFI44L, IFI44, IFI27, MX1, RSAD2 and IFIT1 were considerably upregulated in relation to healthy individuals.
To cite this abstract in AMA style:
Chronopoulou A, Gerochristou M, Raftopoulou S, Stratigos A, Mavragani C. Increased Type I Interferon Inducible Genes Expression in the Peripheral Blood of Patients Presenting Cutaneous Lupus Erythematosus Manifestations [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-type-i-interferon-inducible-genes-expression-in-the-peripheral-blood-of-patients-presenting-cutaneous-lupus-erythematosus-manifestations/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-type-i-interferon-inducible-genes-expression-in-the-peripheral-blood-of-patients-presenting-cutaneous-lupus-erythematosus-manifestations/