Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Adverse social determinants of health (SDoH) are associated with poorer short- and long-term health outcomes. Prior studies have reported considerable prevalence of adverse SDoH in patients with rheumatoid arthritis(RA), but little is known about their impact on achieving disease remission. Thus, we aimed to examine the association between the SDoH and RA disease flare and remission.
Methods: All ≥18-year-old patients within a defined one-county region with incident RA in 1999 -2014 were identified. Incident RA was defined as those who fulfilled the 1987 ACR classification criteria for RA. To estimate adverse SDoH burden, we employed the Social Vulnerability Index (SVI). The SVI considers items across all the SDoH domains and is considered a reliable reflection of a community’s social vulnerability, with a higher index reflecting more vulnerability. Indices of less than 0.25 are considered low vulnerability and those greater than 0.76 are considered high vulnerability. Flare and remission were defined using OMERACT definitions. Flare was defined as a worsening of disease requiring initiation or adjustment of therapy or documentation in the form of statements such as ‘flare up’. Remission was defined as an absence of disease activity (e.g. ‘remission’, ‘quiescent’, ‘no activity’) and/or based on findings of ≤1 tender/swollen joints and normal inflammatory markers. Mixed effects models, accounting for multiple visits, age, sex, RA duration, seropositivity, incidence year, and smoking status, were used to assess the association between flare/remission and SVI. Associations were summarized as odds ratios.
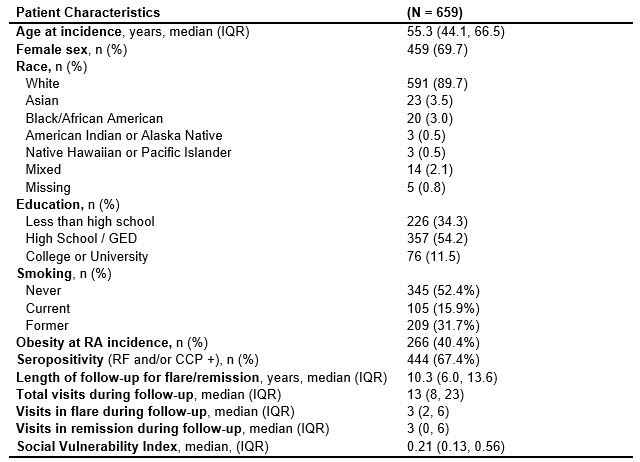
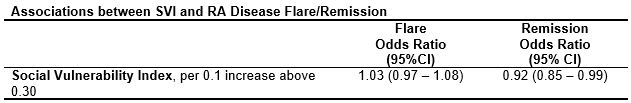
Results: A total of 659 patients with prevalent RA were identified and these patients had a median of 13 follow-up visits over a median of 10.3 years. Patients were a median of 55.3 years old at incidence, 69.7% female, 89.7% white, and 34.3% had less than high school education. Seropositive patients accounted for 67.4% of patients. Further demographics are summarized in table 1. A social vulnerability index was measurable for 642 patients, with a median index of 0.21. At medium-to-high SVIs, further increases in vulnerability were significantly associated with lower likelihood of remission, with 8% lower odds of achieving remission for every 10-percentile increase above an SVI of 0.3 ([OR] 0.92, 95% CI 0.85 – 0.99) (table 2). In terms of disease flare, every 10-percentile increase above an SVI of 0.3 was associated with 3% higher odds of RA flare, but this association did not reach statistical significance (OR 1.03; 95% CI 0.97 – 1.08) (table 2).
Conclusion: Using SVI as a proxy, adverse SDoH burden appears to be associated with lower likelihood of remission. This adds to the existing data on predictors of remission and informs clinicians to consider health-equity interventions to improve outcomes in patients with RA. Further examination in RA cohorts with broader SVI ranges could shed more light on this important topic and would help guide future research towards effective interventions to reduce disparities.
To cite this abstract in AMA style:
Montes D, Myasoedova E, Kodishala C, George R, Hanson A, Kronzer V, Davis J, Crowson C. Increased Social Vulnerability Index Predicts Lower Likelihood of Remission in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-social-vulnerability-index-predicts-lower-likelihood-of-remission-in-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-social-vulnerability-index-predicts-lower-likelihood-of-remission-in-rheumatoid-arthritis-patients/