Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The SARS-CoV2 pandemic reopened the unresolved question of whether and how a viral infection can trigger flares of immune-mediated inflammatory diseases such as systemic lupus erythematosus (SLE). We aimed to analyze the risk of lupus flare after admission for COVID-19.
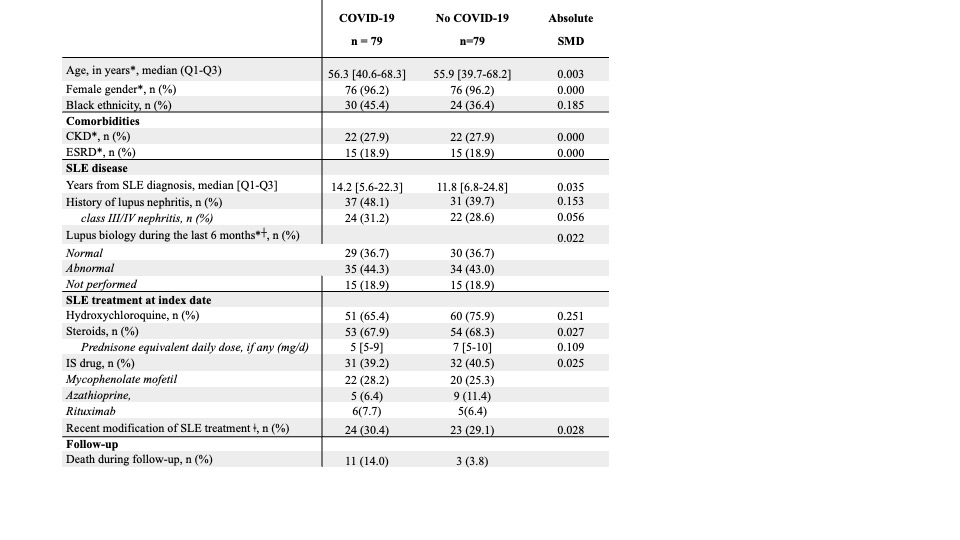
Methods: We performed a matched cohort study using the Assistance Publique – Hôpitaux de Paris Clinical Data Warehouse which collects medical, biological and administrative information from 11 million patients in Paris area. Each SLE patient hospitalized with COVID-19 between March 2020 and December 2021 was matched to one SLE control patient on age ±3years,gender,chronickidneydisease,end-stage renal disease, and lupus biology. The main outcome was a lupus flare during the 6 months follow-up. A flare was considered if a) documented by the treating physician and b) justifying a change in SLE treatment. The electronic health records were individually checked for data accuracy.
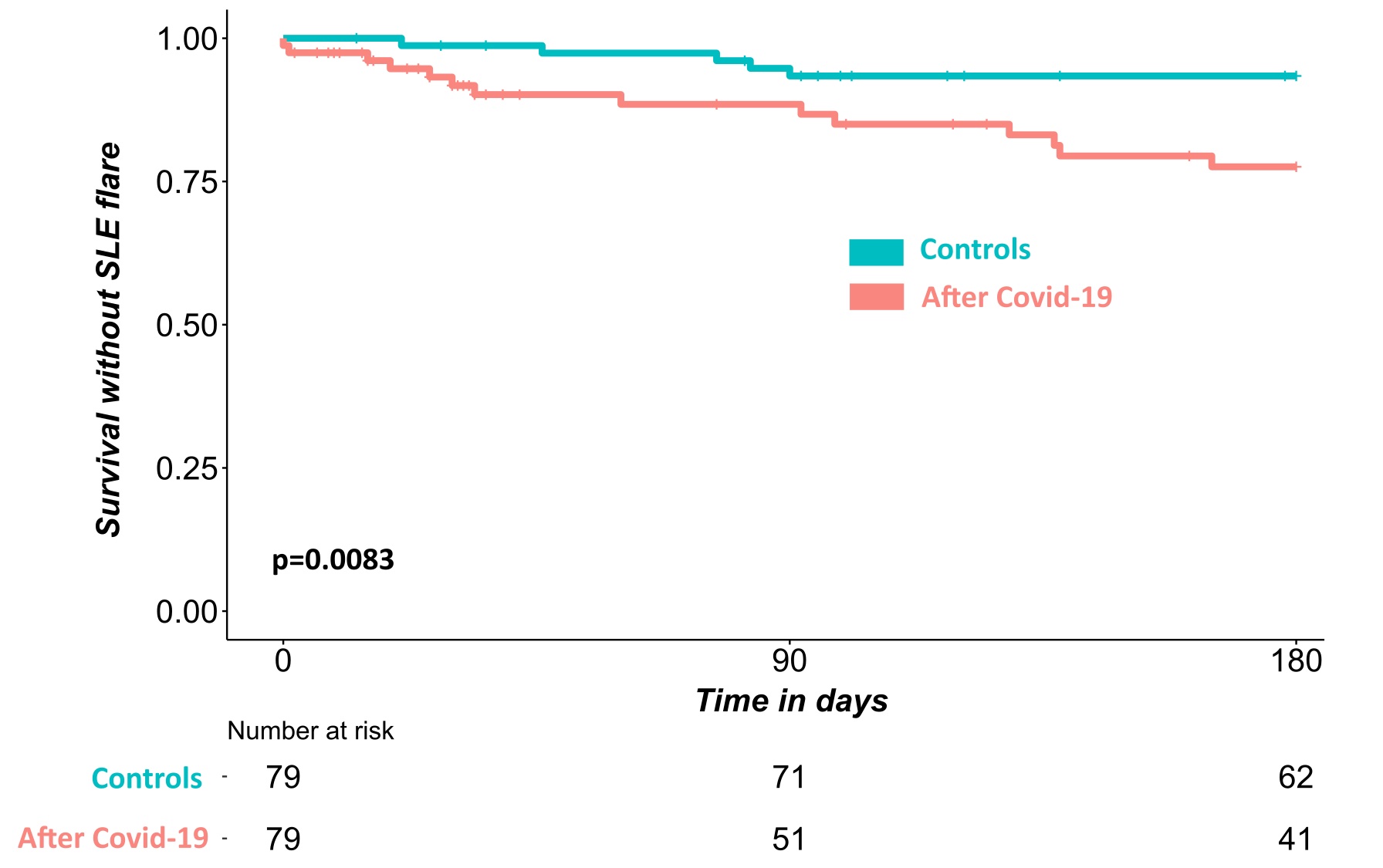
Results: Among 4,533 SLE patients retrieved from the database, 81 have been admitted for a COVID-19 between March 2020 and December 31, 2021 from whom 79 (n=79/81,97.5%) were matched to 79 unique unexposed SLE patients (Table 1). A flare occurred in 14 (17.7%) SLE patients from the COVID-19 group as compared to 5 (6.3%) in the unexposed control group, including 4 lupus nephritis in the exposed group and 1 in the control group. After adjustment for HCQ use at index date and history of lupus nephritis, the risk of flare was higher in exposed SLE patients (hazard ratio [95% confidence interval] of 3.79 [1.49-9.65]).
Conclusion: COVID-19 increases the risk of lupus flare.
Q1: first quartile; Q3: third quartile; CKD: Chronic kidney disease defined as an eGFR < 60mL/min and no end-stage renal disease; ESRD: End-stage renal disease defined as chronic dialysis or renal transplantation; IS: immunosuppressive; SMD: standardized mean differences.
Lupus nephritis classes refer to the ISN/RPSWG classification (25).
┼C3 levels and anti-dsDNA IgG titers measured in the serum at the latest 6 months prior the index date were considered. When performed, lupus biology was defined as either normal – when both C3 level and anti-dsDNA IgG titer were into the normal range – or abnormal – when C3 level was low and/or anti-dsDNA IgG titer was high.
* Matching variables. ǂ SLE treatment modification during the six months before the index date or during COVID episode.
P value was calculated with the log rank test.
To cite this abstract in AMA style:
Mageau A, Gerardin C, Sallah K, Timsit J, Papo T, Sacre K. Increased Risk of Systemic Lupus Erythematosus Flare After COVID-19 [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/increased-risk-of-systemic-lupus-erythematosus-flare-after-covid-19/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-systemic-lupus-erythematosus-flare-after-covid-19/