Session Information
Date: Monday, November 13, 2023
Title: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitides (AAVs) are a group of multisystem inflammatory diseases. One of the most serious and common side-effects of GC and immunosuppressant drug use is infection. No studies have explained the change in risk over time. What’s more, findings from previous studies may not accurately represent the risk of infection due to AAV as many studies are based on hospitalized patients, small sample sizes, prevalent cohorts, different approaches to defining AAV, and/or limited adjustment of potential confounders. To address these research gaps, we conducted a large population-based study of all patients with incident AAV. We aimed to answer three questions: a) what is the independent risk of first severe infection due to AAV, b) the trajectory of the risk for severe infection in AAV compared to the matched controls , and c) the trajectory of the rate of repeated severe infections in AAV compared to the matched controls.
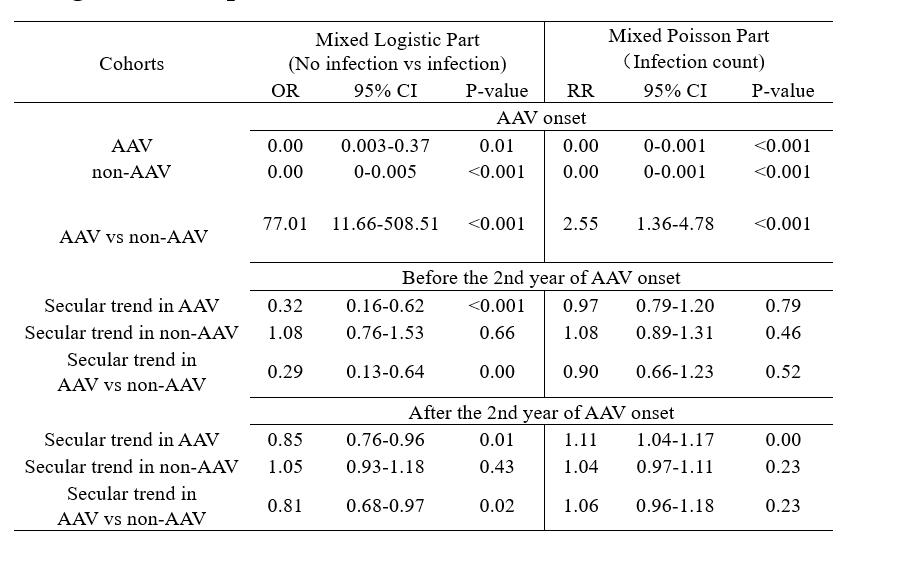
Methods: We conducted an age- and sex-matched cohort study of all patients with incident AAV using administrative health data from British Columbia, Canada. The primary outcome was the first severe infection after AAV onset necessitating hospitalization or occurring during hospitalization. We used multivariate Cox proportional hazard models to compare time to the onset of infection and estimate hazard ratios. The secondary outcome was the longitudinal counts of severe infection. We used two-part zero-inflated Poisson mixed model (ZIPMM) with splines to assess the secular trend in the infection count.
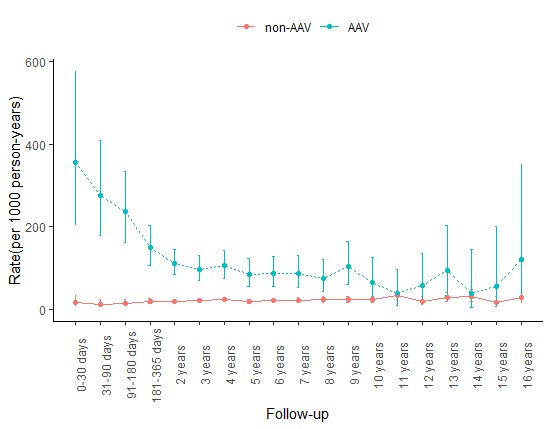
Results: One in three patients with newly diagnosed AAV developed severe infection (3.8-fold when compared to non-AAV).AAV patients had the highest risk of severe infection during the first 30 days of diagnosis, which dropped at different rates before and after the second year. However, among those at risk for severe infections, the rate of repeated severe infections stayed the same over time within the first two years of AAV diagnosis and even increased over time afterward.
Conclusion: In summary, this is the first large comprehensive population-based study evaluating the risk of infection with incident AAV. Our study demonstrates that one in three AAV patients developed severe infections, demonstrating that the diagnosis of AAV is an independent risk factor for severe infection. ZIPMM spline model suggests that an AAV patient who has experienced infection should be treated differently and properly from one who experiences no infection. Having a more precise understanding of which individuals are likely to experience infection and develop repeated infections could help to ensure a more efficient use of healthcare dollars and perhaps a more accurate attribution of intervention effects. This research is a further step towards a deeper understanding of the prevention, screening and treatment of infection over time. We recommend a closer surveillance for severe infections in AAV patients and routine risk checks for severe infections for AAV patients after diagnosis. Further studies are also warranted to further clarify the relative contribution of inflammation and medication, and to identify modifiable risk factors for infections in AAV.
To cite this abstract in AMA style:
Zhao K, Avina-Zubieta J, Xie H, Dehghan N, Esdaile J. Increased Risk of Severe Infection in Patients with Antineutrophil Cytoplasmic Antibody-associated Vasculitides: A Population-based Trend Analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/increased-risk-of-severe-infection-in-patients-with-antineutrophil-cytoplasmic-antibody-associated-vasculitides-a-population-based-trend-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-severe-infection-in-patients-with-antineutrophil-cytoplasmic-antibody-associated-vasculitides-a-population-based-trend-analysis/