Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) are at an increased risk for developing coronary artery disease (CAD) compared to their cohorts without lupus. There have been several studies published that suggest that the presence of lupus nephritis (LN) is independently associated with CAD. However, none of these studies have looked at this association by class of LN. The purpose of our study was to define the characteristics of patients with SLE seen at the University of North Carolina Hospitals (UNCH); assess whether the presence of LN is independently associated with CAD; and evaluate whether this association varies according to specific LN classes.
Methods: A retrospective cross-sectional analysis was performed using medical records of patients 18 years and older with SLE at UNCH from April 4, 2014 to December 31, 2017. Subjects were identified using ICD-9 and ICD-10 codes specific for SLE. LN class was defined by ISN/RPS classification and determined based on review of renal biopsy and clinic notes. CAD was the outcome of interest and was defined by ICD codes for unstable angina, ST segment elevation myocardial infarction (STEMI), or non-STEMI. To determine the association between LN and CAD among SLE patients, logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CI).
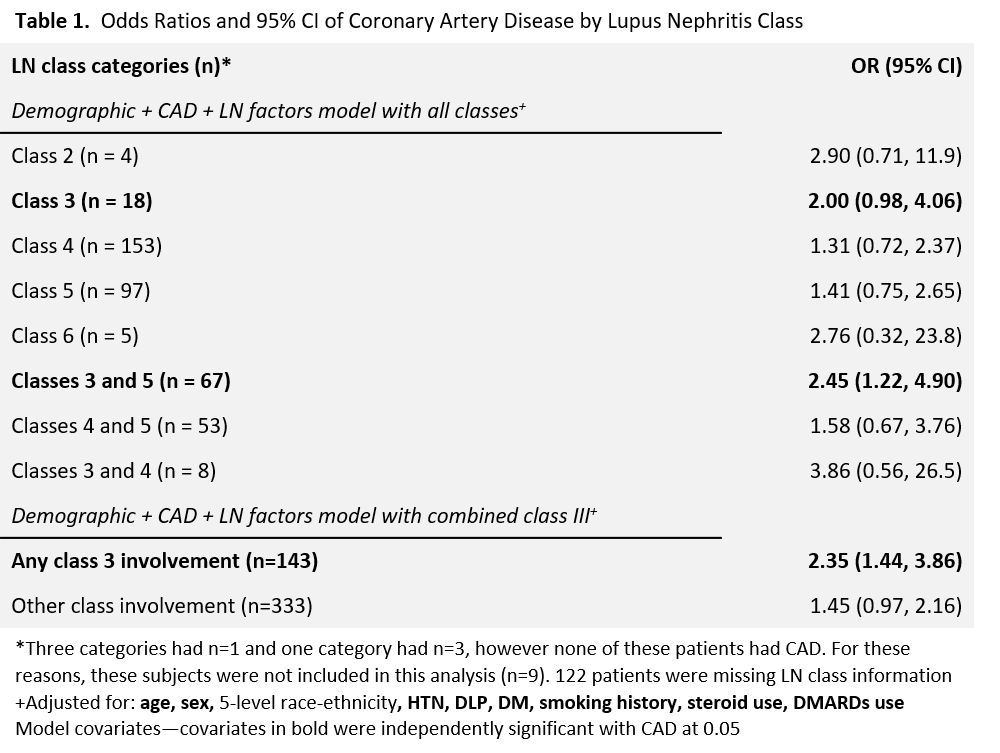
Results: The sample consisted of 3732 patients, 12% men with a mean (standard deviation) age of 48 (15.2) years; 43% White, 38% Black. Seventy percent had hypertension (HTN), 42% had dyslipidemia (DLP), 23% had diabetes mellitus (DM), and 38% had a history of smoking. Sixteen percent had LN (n=598) and 14% had CAD. When adjusting for age, sex, race/ethnicity, HTN, DLP, DM, smoking, steroid use, and disease-modifying antirheumatic drugs (DMARDs) use, the odds of having CAD were significantly higher for SLE patients with LN compared to patients without LN [OR 1.58, 95% CI (1.18, 2.14)]. In the LN analyses (Table 1), combined class III and V was significantly associated with CAD and class III alone was strongly associated with CAD. In several statistical models, class III was either strongly or significantly associated with increased risk of CAD. To better study the relationship between class III LN and CAD, all subjects with evidence of class III LN either alone or in combination were combined and the odds of CAD assessed. In this analysis any class III involvement was significantly associated with CAD compared to subjects without LN.
Conclusion: The results of our study confirm the findings of previous studies that LN is significantly associated with CAD after controlling for demographic, CAD, and lupus-specific factors. Ours is the first to study this association by LN class. We have shown that there may be an unexplored association between class III LN and CAD. We believe that our study reveals a critical area of further investigation and potential clinical intervention.
To cite this abstract in AMA style:
Sun EY, Alvarez C, Sheikh SZ. Increased Risk of Coronary Artery Disease Among Patients with Class III Lupus Nephritis: A Retrospective Study of Patients at the University of North Carolina at Chapel Hill [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/increased-risk-of-coronary-artery-disease-among-patients-with-class-iii-lupus-nephritis-a-retrospective-study-of-patients-at-the-university-of-north-carolina-at-chapel-hill/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-coronary-artery-disease-among-patients-with-class-iii-lupus-nephritis-a-retrospective-study-of-patients-at-the-university-of-north-carolina-at-chapel-hill/