Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose : Renal lesions have been
described in patients with antiphospholipid antibodies (aPL), however their
associations with aPL are inconsistent among studies. Therefore our objective
was to investigate associations between aPL and renal lesions among SLE
patients.
Methods : Studies were selected if they determined
the association between aPL and acute (thrombotic microangiopathy including
“glomerular thrombosis” and “intra-renal thrombosis”) and/or chronic (e.g.
fibrous intimal hyperplasia, focal cortical atrophy) vascular renal lesions in
SLE patients and if aPL-negative patients were included for comparison. Data
sources were Pubmed, Embase, Cochrane Library, hand search, congress abstracts,
and reference lists of studies, without language restrictions. Risk estimates were
independently extracted by 2 investigators. Pooled effect estimates were obtained
by using the Mantel-Haenszel method (random effects).
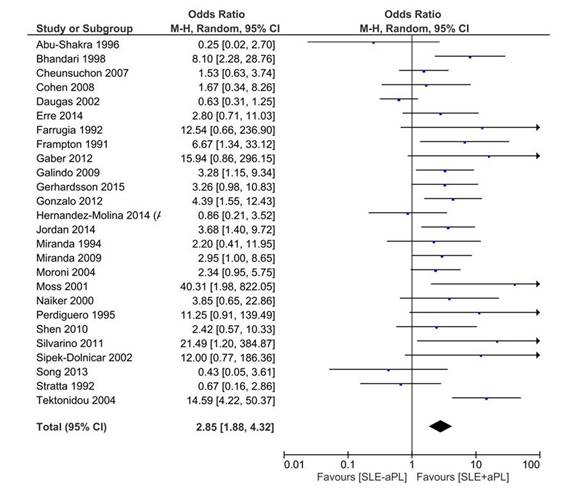
Results: Of 1820 identified records,
25 published studies and 1 abstract (5 cohorts, 5 case-control, 16
cross-sectional) met inclusion criteria, including 2128 SLE patients according
to ACR criteria and 482 cases of renal lesions. Prevalence of renal lesions in
aPL-positive vs. aPL-negative SLE patients was 31.9% (n=243/761) vs. 17.5% (n=239/1367),
respectively. Compared with SLE patients without renal lesions, the overall
pooled odds ratios (OR) for renal lesions in aPL-positive SLE patients was 2.85
(95% confidence interval [CI], 1.88-4.32) (Figure 1). The risk of renal lesions
was the highest for lupus anticoagulant (LA) (9 studies, OR=4.70 [95% CI, 2.36-9.36])
and IgG anticardiolipin antibodies (aCL) (4 studies, OR=3.13 [95% CI, 1.09-8.98])
while IgM aCL (2 studies, OR=1.51 [95% CI, 0.03-88.59]) and anti-β2-glycoprotein
I antibodies (aβ2GPI) (4 studies, OR=1.66 [95% CI, 0.54-5.11] did
not reach statistical significance. Furthermore, among all aPL assays, LA was
the only test to be significantly associated with both acute (4 studies, OR=2.89
[95% CI, 1.10-7.60]) and chronic renal lesions (2 studies, OR for LA=3.56 [95%
CI, 1.05-12.08]).
Conclusion : In SLE patients,
aPL-positivity is associated with a significant 3- to 5-fold increased risk for
renal lesions. This risk is mainly driven by LA and IgG aCL. While acute thrombotic
renal lesions are known to be associated with aPL, our findings suggest that
chronic renal lesions could be associated with aPL but with a lower level of
evidence.
Figure 1
To cite this abstract in AMA style:
Domingues V, WAHL D, Zuily S. Increased Risk of Acute and Chronic Renal Lesions Associated with Antiphospholipid Antibodies in Patients with Systemic Lupus Erythematosus: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/increased-risk-of-acute-and-chronic-renal-lesions-associated-with-antiphospholipid-antibodies-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-acute-and-chronic-renal-lesions-associated-with-antiphospholipid-antibodies-in-patients-with-systemic-lupus-erythematosus-a-systematic-review-and-meta-analysis/