Session Information
Date: Sunday, November 13, 2022
Title: Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Optimizing jSLE management is crucial to prevent flares as the damage sustained during flares contributes to lifelong morbidity and mortality. The onset of the SARS-CoV-2 pandemic in New York in March of 2020 disrupted routine care, and the few studies on jSLE at the time reported an increase in flares. As data on jSLE was limited, this study sought to increase the information about disease activity among these patients during the SARS-CoV-2 pandemic. The primary objective was to compare the population flare rate between 2 time periods: March 1, 2019 to February 29, 2020 (pre pandemic period), and March 1, 2020 to March 1, 2021 (post pandemic period). The secondary objective was to assess for differences in factors associated with disease flares in the 2 time periods.
Methods: This was a retrospective, chart review at a single center in New York. The study population included male and female patients < 21 years old seen between March 1, 2020 and June 1, 2020, and had at least one visit between March 1, 2019 and February 29, 2020. They were < 18 years old at diagnosis and met the ACR 2011 SLE criteria. Demographic information, the number of flares, the number of contacts with the medical team (office visits, virtual visits, telephone calls, and secure electronic medical record messaging), medication adherence, and healthcare utilization (number of doctor visits, emergency department visits, and hospitalizations) were recorded.As there was concern that patients could not obtain labs during the SARS-CoV-2 pandemic, validated measures of SLE were unobtainable, so physician documentation of a flare was used as the flare measure. Medication adherence was defined as medication availability of > 80% per EMR refills compared to documented medication regimens. Descriptive statistics including frequencies, percentages, medians, interquartile ranges, means, and standards deviations were performed and reported.
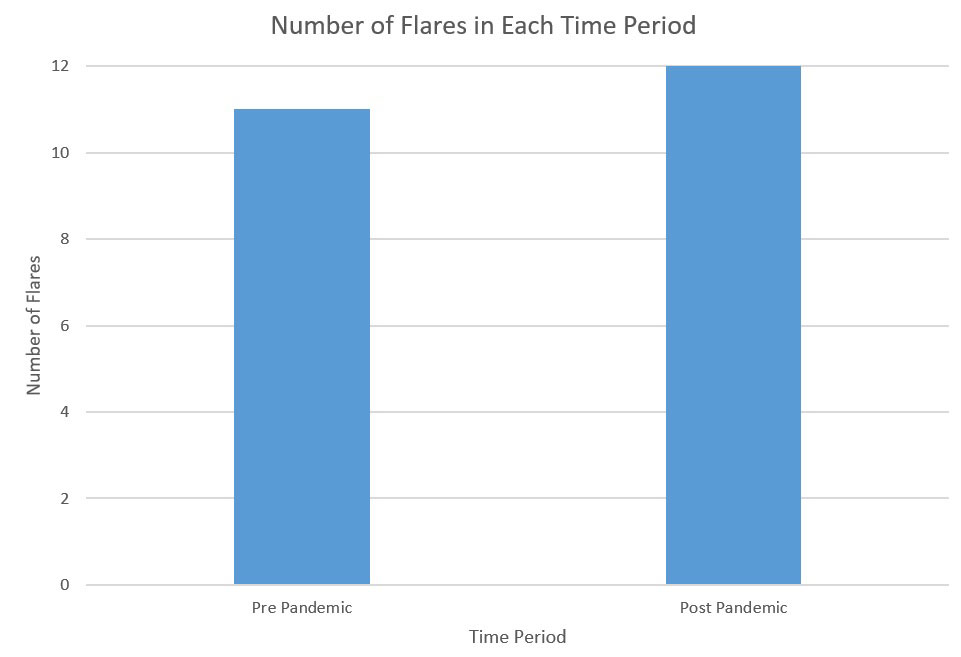
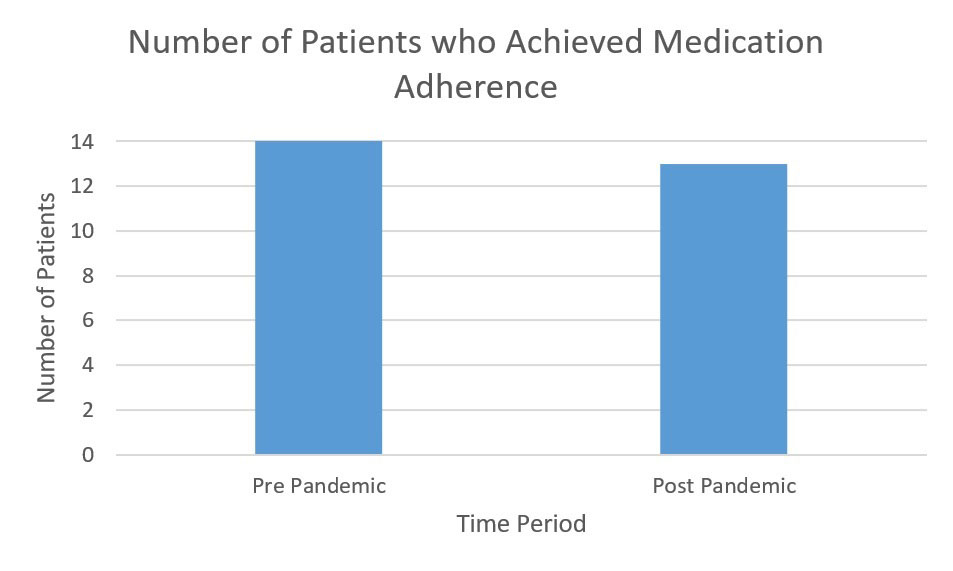
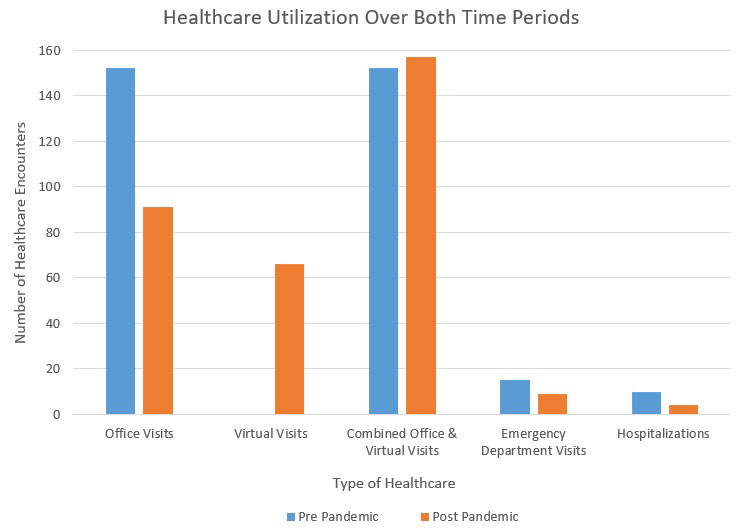
Results: A similar number of flares occurred in both periods: 11 and 12 in the pre and post pandemic period. In each period, 3 flares led to 3 hospitalizations. Medication adherence was stable with 14 and 13 patients achieving medication adherence in the pre and post pandemic periods. Medication adherence was better among patients on more medications in both periods. There was a 12% increase in patient and medical team contact in the post pandemic period. The number of doctor visits remained stable: 152 in the pre pandemic period (all in person) and 157 in the post pandemic period (91 in person and 66 virtual). Emergency department visits and hospitalizations decreased in the post pandemic period: 15 to 9 and 10 to 4.
Conclusion: In contrast to other studies, the flare rate was similar in the pre and post pandemic periods. Notably there was a rapid acceptance and utilization telemedicine so that total doctor visits remained unchanged. Increased contact between patients and the medical team using traditional and non-traditional methods may help to stabilize patient outcomes, potentially through improved medication adherence. However, this is a single center experience and the results may not be generalizable. Further studies are needed to evaluate the possibility that increased contact with patients increases medication adherence.
To cite this abstract in AMA style:
Fennell J, Jannat-Khah, DrPH, MSPH D, onel k. Increased Patient Contact May Mitigate Flares Among jSLE Patients [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/increased-patient-contact-may-mitigate-flares-among-jsle-patients/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-patient-contact-may-mitigate-flares-among-jsle-patients/