Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Resistant hypertension (RHTN) is associated with increased risk of cardiovascular events in the general population. Patients with systemic lupus erythematous (SLE) have increased cardiovascular risk, but little is known about RHTN in patients with SLE. We first compared the risk of RHTN in SLE patients and matched controls, then defined factors associated with RHTN in SLE, and finally calculated the risk of mortality associated with RHTN in SLE.
We used a validated algorithm (94% PPV) to identify adults with SLE from de-identified electronic health records at an academic medical center. We established a control cohort matched by age, race, and sex, with a 5:1 control-case ratio. Follow-up began with first SLE ICD9 code (cases) or first ICD9 code (controls) and continued until RHTN or last visit. A RHTN diagnosis required simultaneous use of 3 antihypertensives including a thiazide diuretic and a mean outpatient blood pressure ≥140/90 in the 6 months after therapy, or simultaneous use of ≥4 antihypertensives.
We extracted demographic and comorbid variables using computer programming and included values closest to a patient’s first relevant ICD9 code. We defined end-stage renal disease (ESRD) by an ESRD ICD9 or dialysis CPT code. We ascertained mortality by Social Security death files and hospital records. We used Cox proportional hazards models to compare risk of RHTN between groups, in incident cases only.
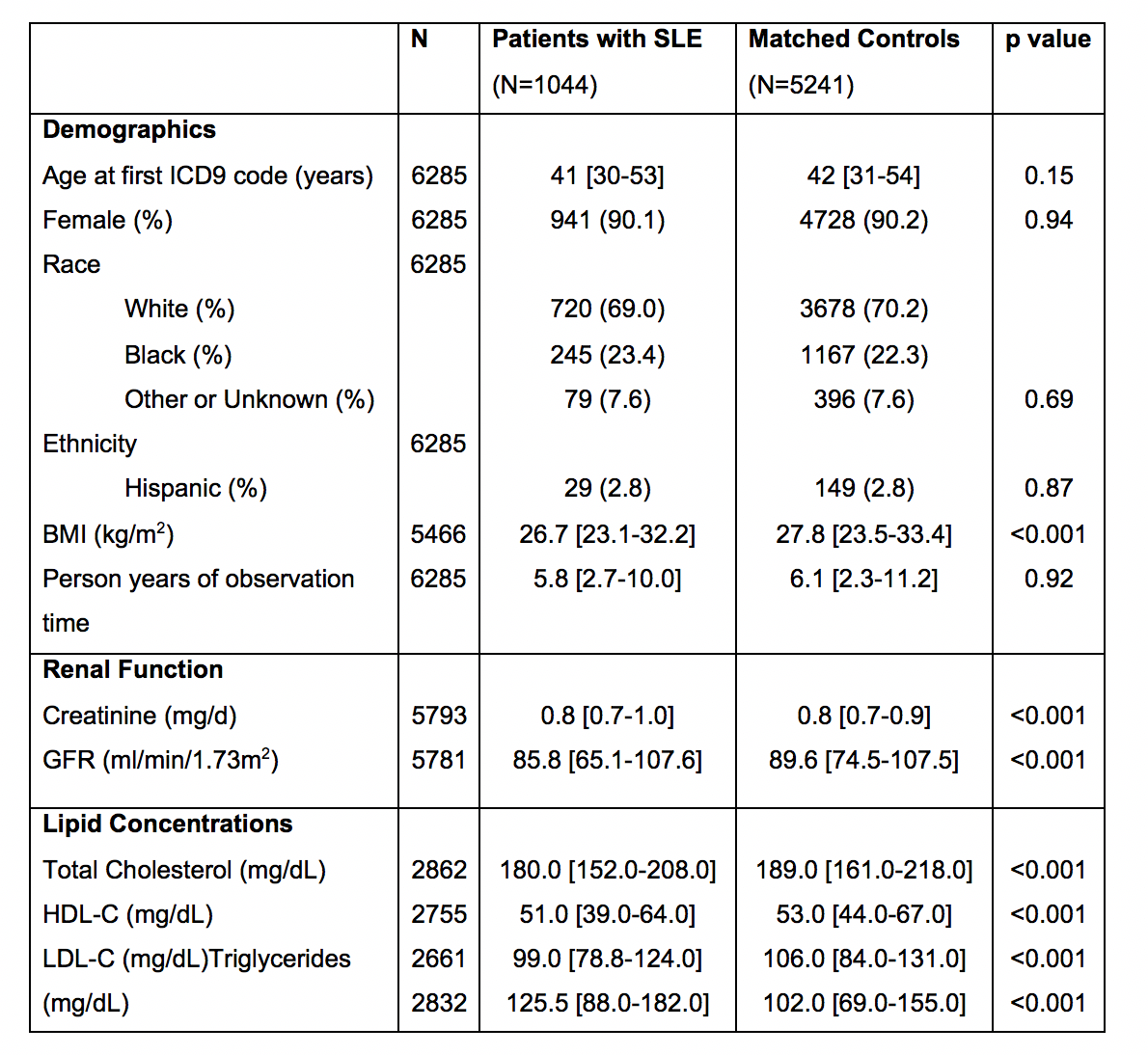
We studied 1044 SLE patients and 5241 control subjects (Table). RHTN developed in 106 SLE patients (10%) and 278 controls (5%), with an incidence rate of 14.7 cases/1000 person-years in SLE compared to 7.4 in controls [HR 1.66, 95% CI, 1.26-2.21] (Figure). Patients with SLE had a higher risk of RHTN after adjustment for age, sex, race, calendar year, creatinine, and ESRD [HR 1.50, 1.12-2.00]. Among these patients, black race [HR: 3.20 CI: 2.48–4.12] and ESRD [HR: 5.76 95% CI: 3.85–8.62] were associated with RHTN. Finally, 25% of SLE patients with RHTN died compared to 10% of SLE patients without RHTN; this association remained significant after adjustment for age, sex and race [HR 2.83 CI: 1.65–4.87].
SLE Patients have a 1.7-fold higher risk of developing RHTN compared to frequency-matched controls. RHTN is an important comorbiditiy for clinicans to recognize in SLE, as it is associated with a 2.8-fold higher mortality risk.
Table. Baseline Characteristics
^Chi-squared tests were used for categorical variables; Wilcoxon-rank sum for continuous. p<0.05 considered significant. Values are shown as median [IQR] or n (%).
Figure. Cumulative Incidence of RHTN
To cite this abstract in AMA style:
Gandelman JS, Khan OA, Shuey M, Neal JE, Dickson A, Barnado A, Wang L, Dupont W, Stein CM, Chung CP. Increased Incidence and Prevalance of Resistant Hypertension in Patients with Systemic Lupus Erythematosus: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/increased-incidence-and-prevalance-of-resistant-hypertension-in-patients-with-systemic-lupus-erythematosus-a-retrospective-cohort-study/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-incidence-and-prevalance-of-resistant-hypertension-in-patients-with-systemic-lupus-erythematosus-a-retrospective-cohort-study/