Session Information
Date: Tuesday, November 10, 2015
Title: Reproductive Issues in Rheumatic Disorders: Basic and Clinical Aspects Poster Session
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Although adverse obstetrical complications are more frequent in SLE
women, no one has evaluated healthcare costs during SLE pregnancies. Thus, we
aimed to evaluate if SLE pregnancies result in higher direct healthcare cost
components (including physician services during pregnancy and neonatal period,
and delivery-related costs) compared to pregnancies from the general
population.
Methods: We used data from the "Offspring of SLE mothers Registry
(OSLER)" including all women who had ³1 hospitalization for delivery after
SLE diagnosis, identified through Quebec’s healthcare databases (1989-2009) which
provide information on all physician services and hospitalizations in the
province. OSLER also includes a randomly selected control group of women
matched ³4:1 for age and year of delivery. We
determined average physician costs for the SLE and non-SLE pregnancies from
first gestational week until birth and the neonatal period (for both mother and
child) from birth until postnatal gestational age of 44 weeks. We also
estimated average hospitalization costs for the SLE and non-SLE deliveries
(including inpatient physician costs). Costs were normalized to 2014 Canadian
dollars.
We
performed multivariate random effect log-linear and linear regression analyses
to establish whether costs during pregnancy and the neonatal period were
associated with SLE status, adjusting for relevant
covariates.
Results: We identified 509 women with SLE who had 712 deliveries and 5824
controls who had 8363 deliveries during the study period. SLE deliveries
occurred at a lower mean gestational age compared to control deliveries, and
birth weight was lower in SLE offspring as opposed to unexposed offspring
(Table 1). In addition, the maternal length of hospitalization for delivery was
longer for SLE deliveries versus controls (Table 1).
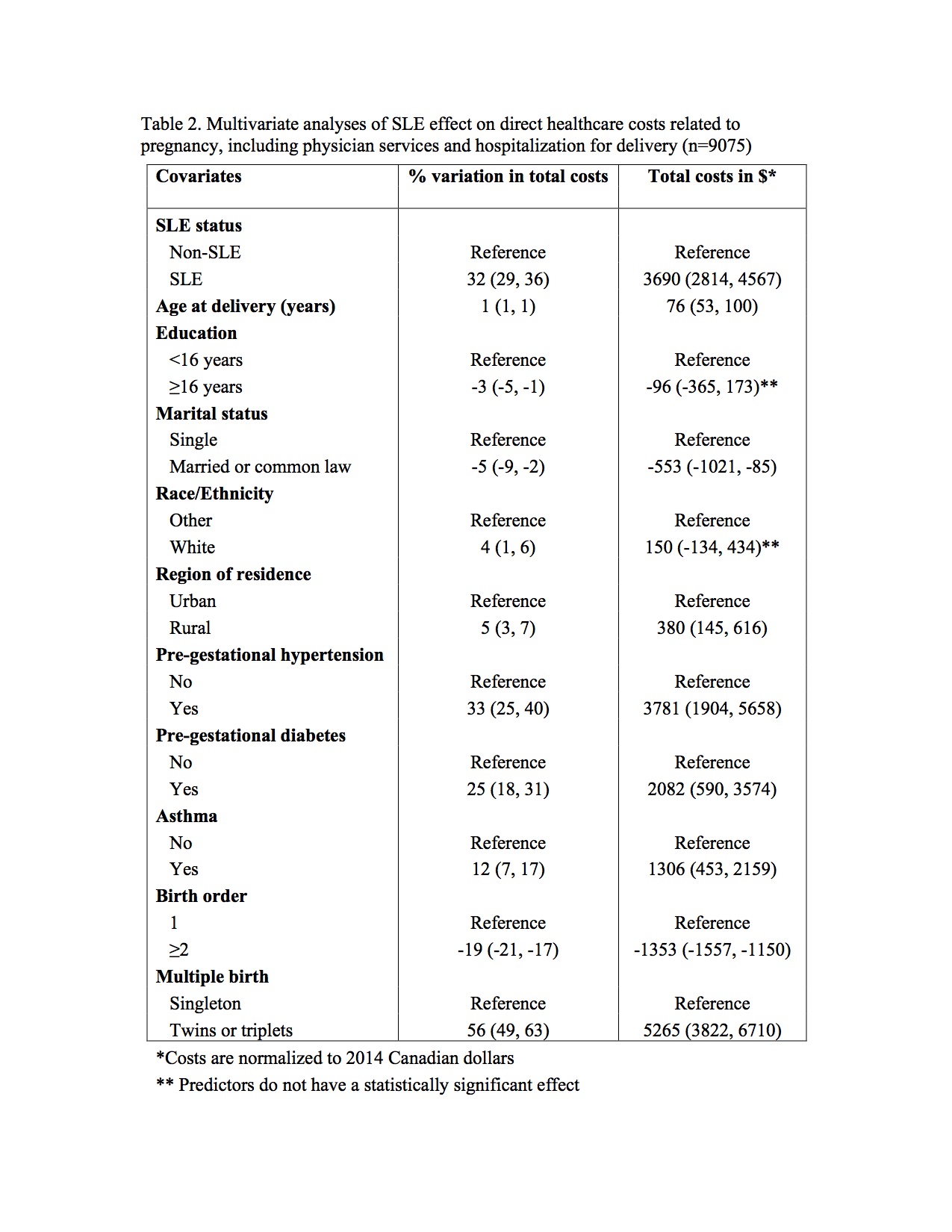
Compared to control pregnancies, we observed substantially higher costs
for both physician services and hospital stays for delivery, resulting in
higher costs for SLE pregnancies [10 833$ vs 6 828$; difference 4 004$ (95% CI 3
300, 4 709)]. In multivariate analyses, SLE pregnancies
had a 32% (95% CI 29, 36) increment in costs, or alternatively a 3 690$ (95% CI 2
814, 4 567) increase in costs, compared to control
pregnancies (Table 2).
Conclusion: Compared to pregnancies from the general population, SLE pregnancies are
associated with substantially higher direct healthcare costs, including costs
for physician services and hospitalization for delivery. Our study is the first
to highlight the economic burden of SLE pregnancies, identifying an area of
heavy healthcare use.
To cite this abstract in AMA style:
Moura C, Bernatsky S, St. Pierre Y, Scott S, Pineau CA, Clarke AE, Vinet E. Increased Direct Healthcare Costs in SLE Pregnancies [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/increased-direct-healthcare-costs-in-sle-pregnancies/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-direct-healthcare-costs-in-sle-pregnancies/