Session Information
Date: Monday, November 14, 2022
Title: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes II: Imaging
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Pain is a hallmark feature of psoriatic arthritis (PsA); however, its apparent multi-factorial nature makes it difficult for rheumatologists to assess and manage. Clinically, nociplastic processes appear to contribute to the PsA pain experience, as shown by frequent co-existing fibromyalgia (FM), a prototypical nociplastic pain disorder [1,2]. Yet there are no objective data to corroborate this observation. This is important to determine given the distinct nociplastic pain management compared to classical anti-inflammatory PsA therapies. Nociplastic pain is characterised by amplified central nervous system responses and altered functional brain connectivity demonstrated in several neuroimaging studies. In particular, the insular cortices (IC), which are the key sensory integrative hubs that capture and compute distinct dimensions of pain perception, have consistently displayed increased connectivity in several nociplastic pain conditions [3-6]. This is the first study to investigate such objective neurobiological markers of nociplastic pain in PsA.
Methods: PsA patients with active disease who fulfilled CASPAR criteria [7] were clinically characterised. Nociplastic pain was assessed using the ACR 2011 FM Survey criteria [8] before undertaking a 6-minute functional MRI scan. Images were acquired by a 3 Tesla, 32 channel phased array head coil using a T2*-weighted gradient-echo echo-planar imaging pulse sequence. Functional MRI data were analyzed using the functional connectivity CONN toolbox, based on SPM12 and ran on MATLAB R2019b. Bilateral subdivisions of the IC: anterior (ant), middle (mid) and posterior (post) IC, were our selected regions of interest (ROI). ROI to whole brain functional connectivity was estimated for each patient followed by group level multiple linear regression which correlated ROIs connectivity to our measure of nociplastic pain while correcting for age, sex and multiple comparisons (FDR < 0.05). Pearson correlations were additionally conducted (Tab. 1). Clinical data were analysed using simple descriptive statistics.
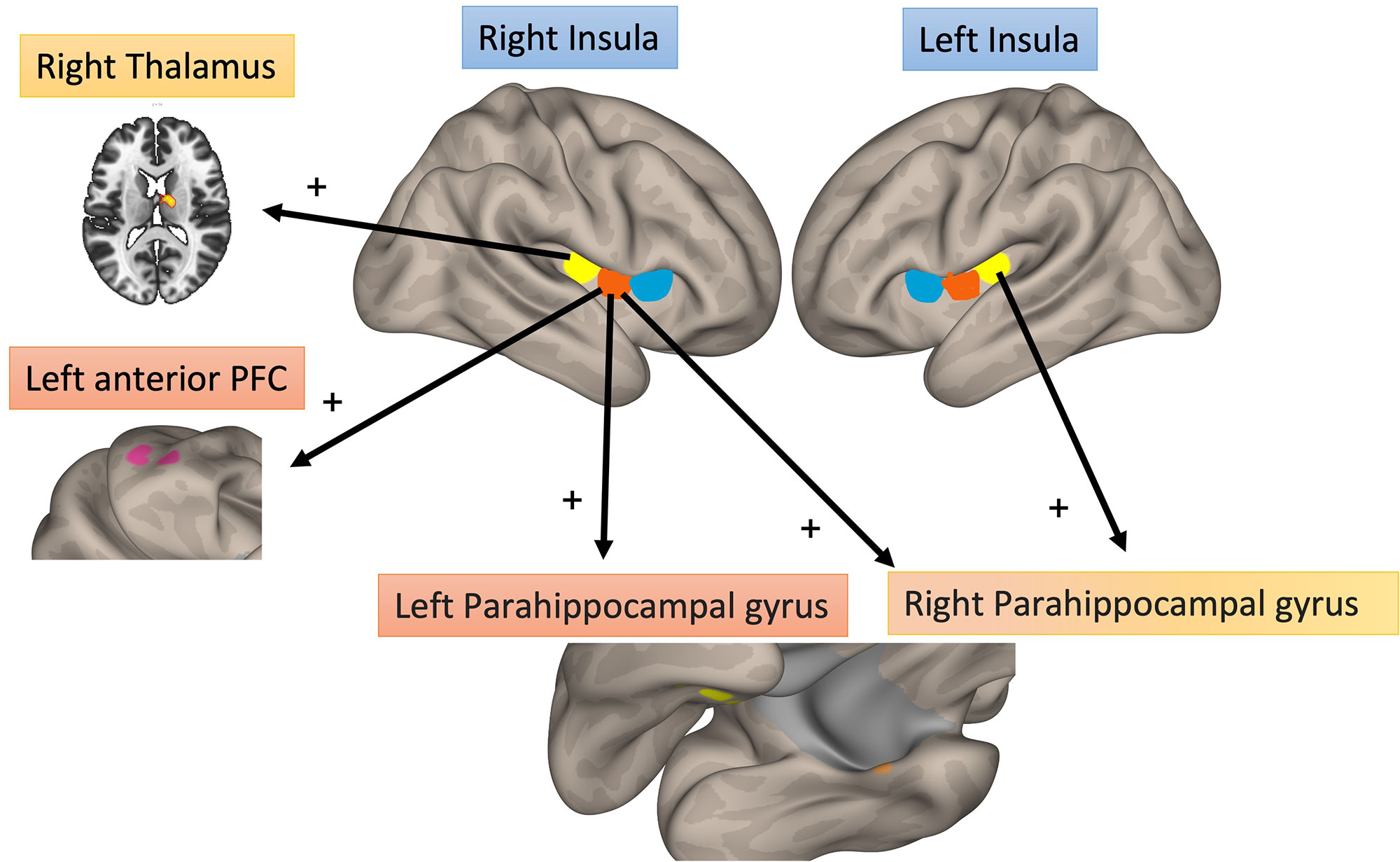
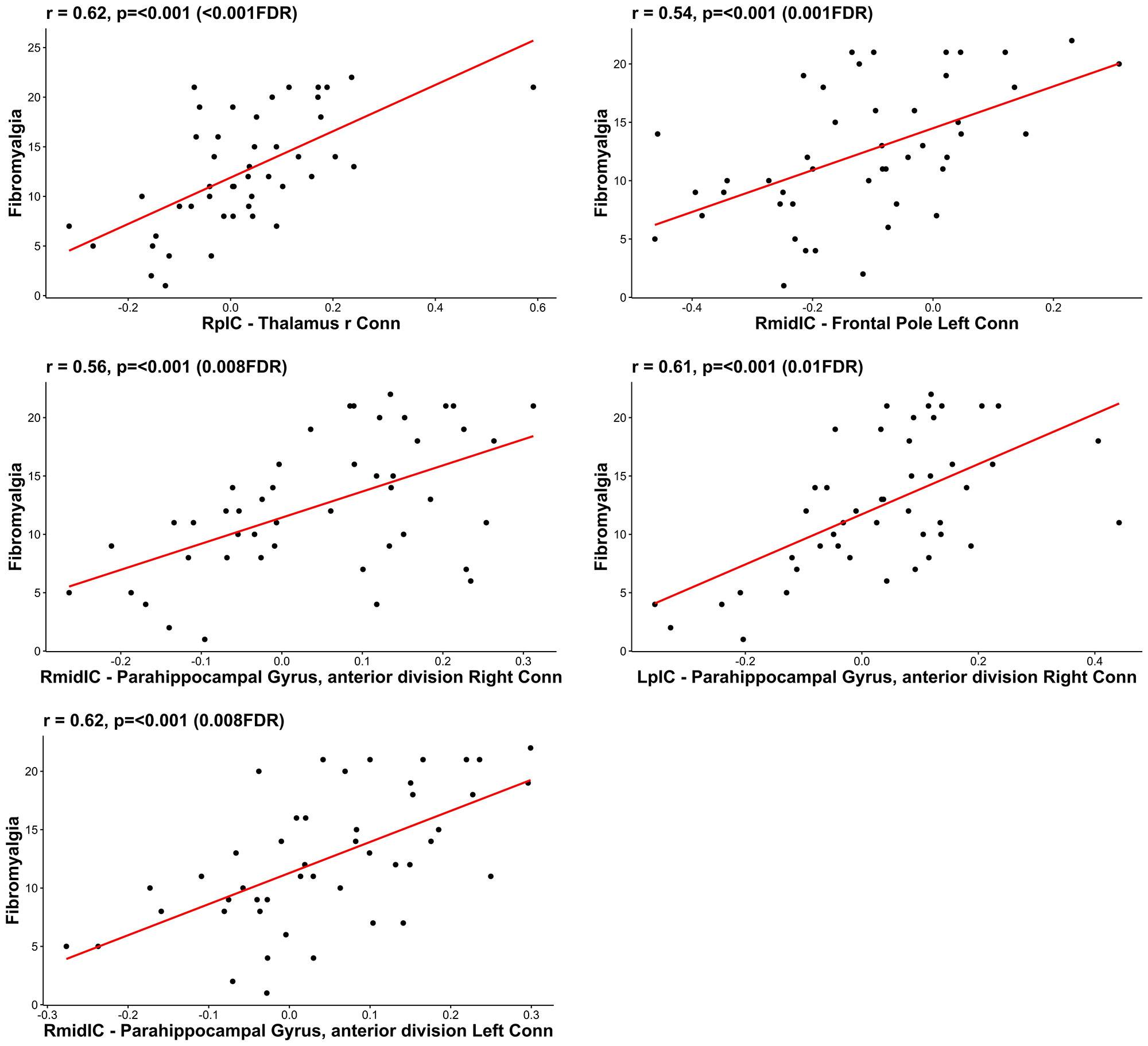
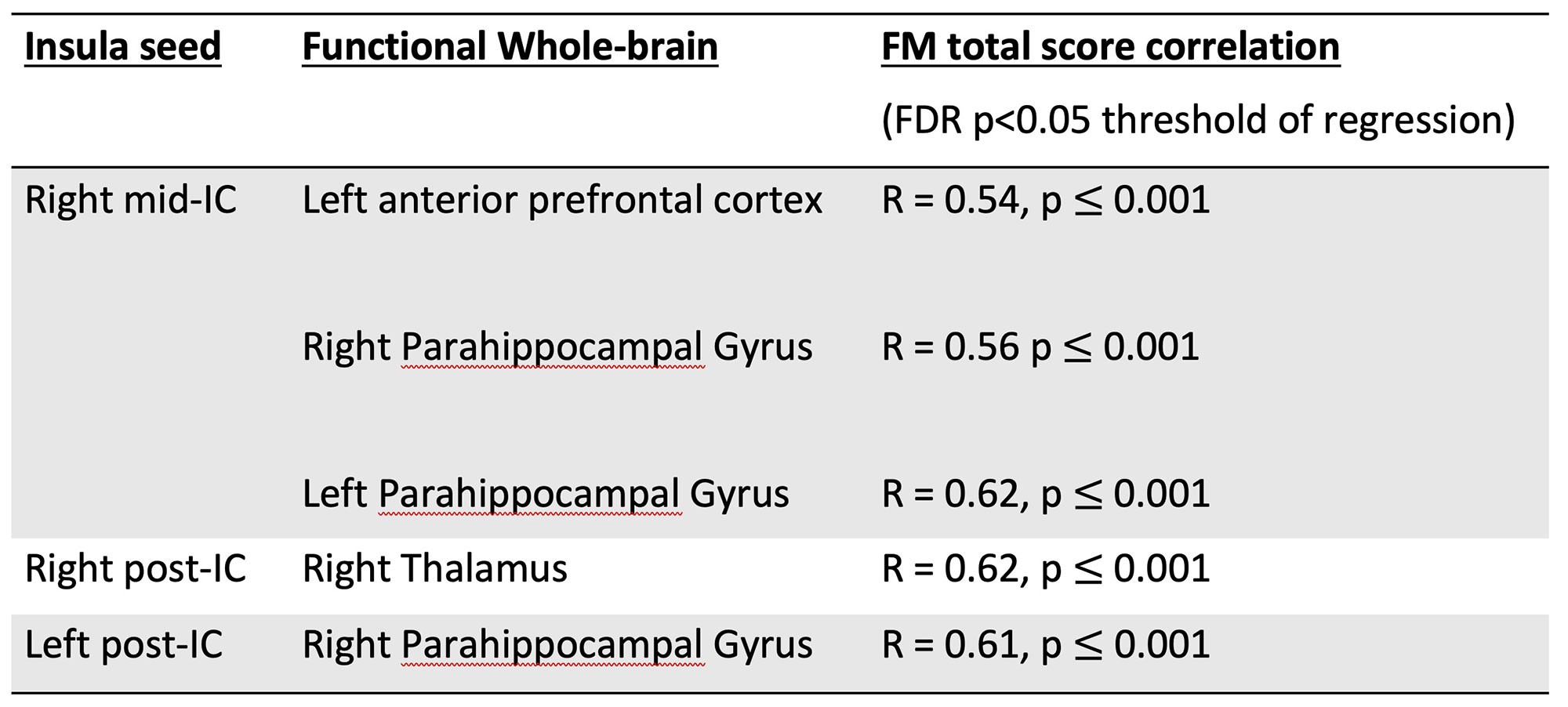
Results: 46 out of 50 patients enrolled, completed the functional MRI scan (mean age 49; 54% female; mean disease duration 7 years; mean ACR FM score 12.6 ±5.9; mean DAPSA 41.8 ±20). Of these, 41% fulfilled FM criteria. PsA patients with higher FM scores displayed increased connectivity between: 1) right mid IC to left anterior prefrontal cortex (R = 0.54, p ≤ 0.001) and bilateral parahippocampal gyrus (right R = 0.56, p ≤ 0.001, left R = 0.62, p ≤ 0.001); 2) right post IC to right thalamus (R = 0.62 p ≤ 0.001); 3) left post IC to right parahippocampal gyrus (R = 0.61, p ≤ 0.001) (Fig.1; Fig.2; Tab. 1).
Conclusion: For the first time, we report neurobiological evidence of nociplastic pain in PsA. Increased functional brain connectivity between the mid-posterior IC (right more than left) and brain areas involved in sensory (thalamus), learning/affective (parahippocampal gyrus), and cognitive (prefrontal cortex) pain modulation is demonstrated. PsA should be considered a mixed-pain state. Rheumatologists should assess for nociplastic pain in PsA and adjust their management approach accordingly.
RpIC – right posterior Insula cortex; RmidIC – right middle Insula cortex; LpIC – left posterior Insula cortex; FDR – False Discovery Rate.
To cite this abstract in AMA style:
Sunzini F, Stefanov K, Al-Wasity S, Harte S, Harris R, Clauw D, Siebert S, Goodyear C, Waiter G, Basu N. Increased Brain Functional Connectivity to the Insula Is Associated with Nociplastic Pain in Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/increased-brain-functional-connectivity-to-the-insula-is-associated-with-nociplastic-pain-in-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-brain-functional-connectivity-to-the-insula-is-associated-with-nociplastic-pain-in-psoriatic-arthritis/