Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Awareness of comorbidity in patients with SLE is increasing. Most studies to date have described comorbidity burden in prevalent SLE. We estimated the incidence of vascular events, – by age and sex, – in a large inception cohort of patients with SLE compared with matched general population controls.
Methods: We assembled a cohort of adult patients registered with a first-time diagnosis of SLE (ICD codes) from January 1996 to July 2018 in the Danish National Patient Register (DNPR). SLE patients were age, – and sex-matched to population controls randomly selected from the Danish Civil Registration System. We used ICD codes from the DNPR to determine the presence of cardiovascular disease (Myocardial Infarction (MI)), cerebrovascular disease (CVD), and peripheral vascular disease (PVD) during outpatient and inpatient care. Individuals with prevalent MI, CVD, and PVD at baseline (SLE diagnosis) were excluded from the analyses of incident events. We estimated incidence rates (IRs), incidence rate ratios (IRRs), and incidence rate differences (IRDs) per 1,000 person-years of MI, CVD, and PVD by sex and age (< 50 years vs ≥ 50 years at baseline) during up to 10 years of follow-up. Analyses were done separately for each disease category, e.g., individuals with incident MI were retained for analyses of CVD and PVD. IRRs and IRDs were adjusted for age and sex using Poisson regression and presented with 95% CIs.
Results: We identified 3,178 patients with incident SLE and 60,090 age- and sex-matched general population comparators. 84% of SLE patients and non-SLE controls were female; the mean age at baseline was 47 years. At baseline, the prevalence of MI (2.9% vs 1.40%), CVD (7.0% vs 2.7%), and PVD (5.5% vs 1.4%) was higher in SLE patients compared with the general population controls.
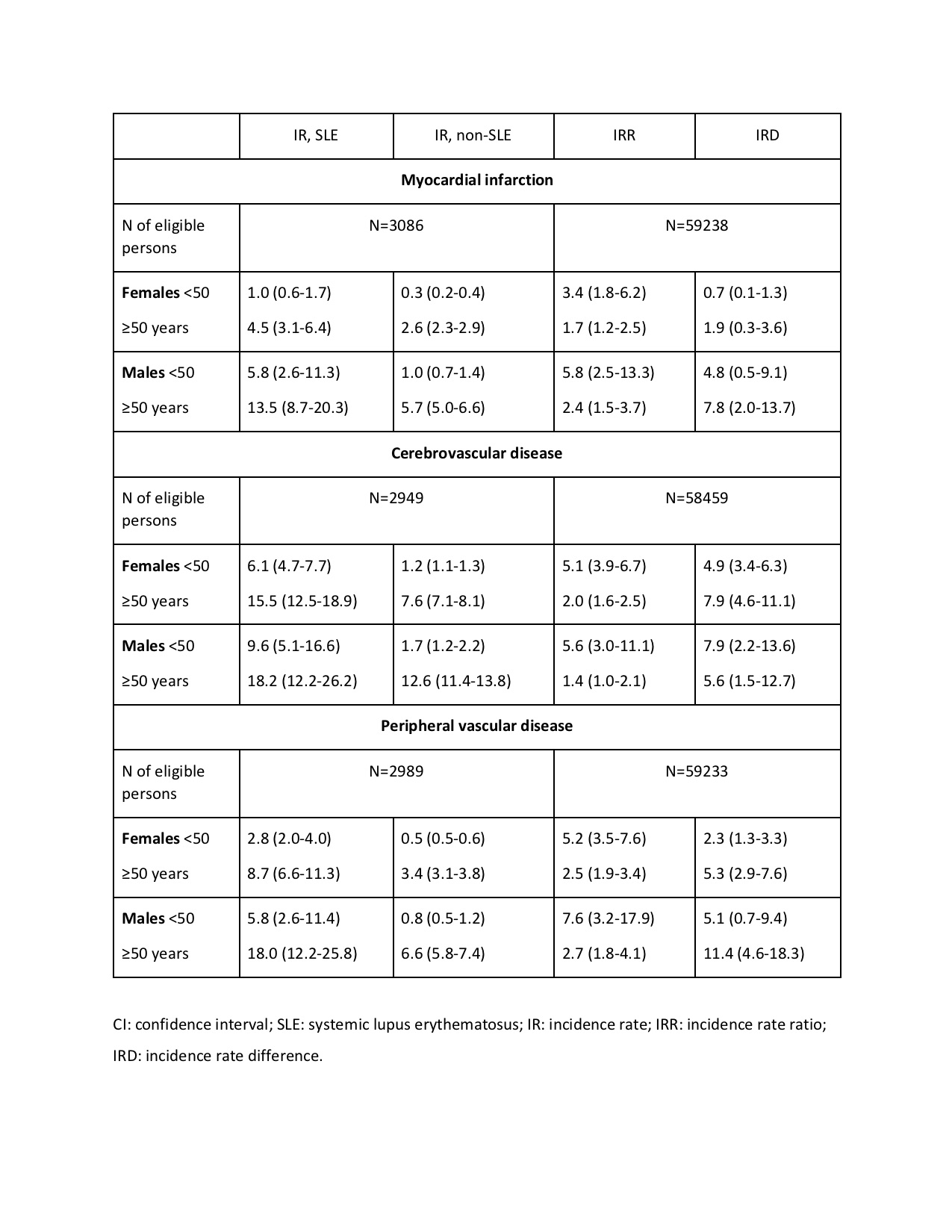
During follow-up, patients with SLE had substantially increased IRs of the above vascular events, with IRRs ranging from 1.7 to 7.6 across sex and age groups (Table 1). Although the absolute rates (IRs) were higher in SLE patients vs controls in the older age group, the IRRs were consistently higher for those aged < 50 at baseline, both females and males. In this age group, female SLE patients had a 5-fold increased risk of CVD and PVD and a 3-fold increased risk of MI. Male SLE patients had an 8-fold increased risk of PVD and a 6-fold increased risk of CVD and MI.
The IRDs ranged from 0.7 (MI in females aged < 50) and 11.4 (PVD in males aged ≥ 50) (Table 1). Interestingly, IRDs were higher in males vs females in both age groups for MI and PVD, and in the younger age group for CVD.
Conclusion: In this nationwide study utilizing prospectively collected registry data, incident patients with SLE were more likely to develop vascular disease than general population controls during up to 10 years of follow-up after SLE diagnosis. This was seen for women and men aged less or more than 50 years at the time of diagnosis but with the highest IRRs of MI, CVD, and PVD in the younger group of SLE patients. Male subjects had a higher incidence of vascular disease, reflected in male SLE patients having the highest IRDs for MI and PVD. Our findings highlight the need for a thorough assessment of vascular comorbidities in SLE patients, at the time of SLE diagnosis and during follow-up, irrespective of sex and age.
To cite this abstract in AMA style:
Baronaite Hansen R, Simard J, Faurschou M, Jacobsen S. Incident Vascular Events in Danish Nationwide Cohort of Patients with Newly Diagnosed Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/incident-vascular-events-in-danish-nationwide-cohort-of-patients-with-newly-diagnosed-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incident-vascular-events-in-danish-nationwide-cohort-of-patients-with-newly-diagnosed-systemic-lupus-erythematosus/