Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
In patients with microscopic polyangiitis (MPA), a variety of pulmonary lesions including diffuse alveolar hemorrhage (DAH), airways disease and interstitial lung disease (ILD) have been reported. Although DAH is a severe complication of MPA, its etiology and prognosis are poorly understood. The purpose of this study was to identify incidence and predictors of DAH and to evaluate its impact on clinical outcome in patients with MPA, focusing on the association of airways disease with DAH.
Methods:
We conducted a multi-center retrospective cohort study of patients with myeloperoxidase anti-neutrophil cytoplasmic antibody (MPO-ANCA) positive MPA at three institutes (Kyoto Prefectural University of Medicine, Japanese Red Cross Kyoto Daiichi Hospital, and Matsushita Memorial Hospital) from January 2006 to June 2015. All patients met the Chapel Hill Consensus Conference definition of MPA. DAH was diagnosed on the basis of bronchoscopy, CT findings, and hemoptysis. We evaluated chest CT images at the onset of MPA and examined the presence of airways disease and ILD. We assessed the associations of airways disease with DAH using odds ratio (OR) and 95% confidence interval (95% CI) estimated from logistic regression adjusted for other baseline characteristics, including age, sex, smoking history, antithrombotic drug use, ILD, rapidly progressive glomerulonephritis (RPGN), nerve involvement, gastrointestinal involvement, the five factor score (FFS), the Birmingham vasculitis activity score (BVAS), MPO-ANCA titer. We compared Kaplan-Meier survival curves between the 2 groups with or without DAH using the log-rank test and hazard ratio estimated by Cox proportional hazards model.
Results:
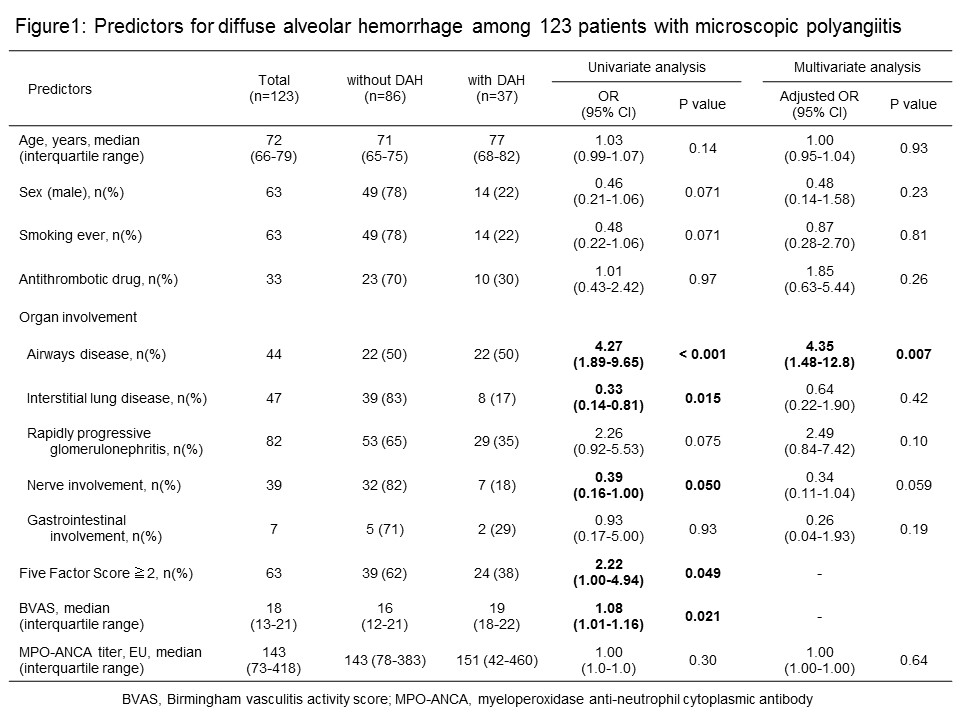
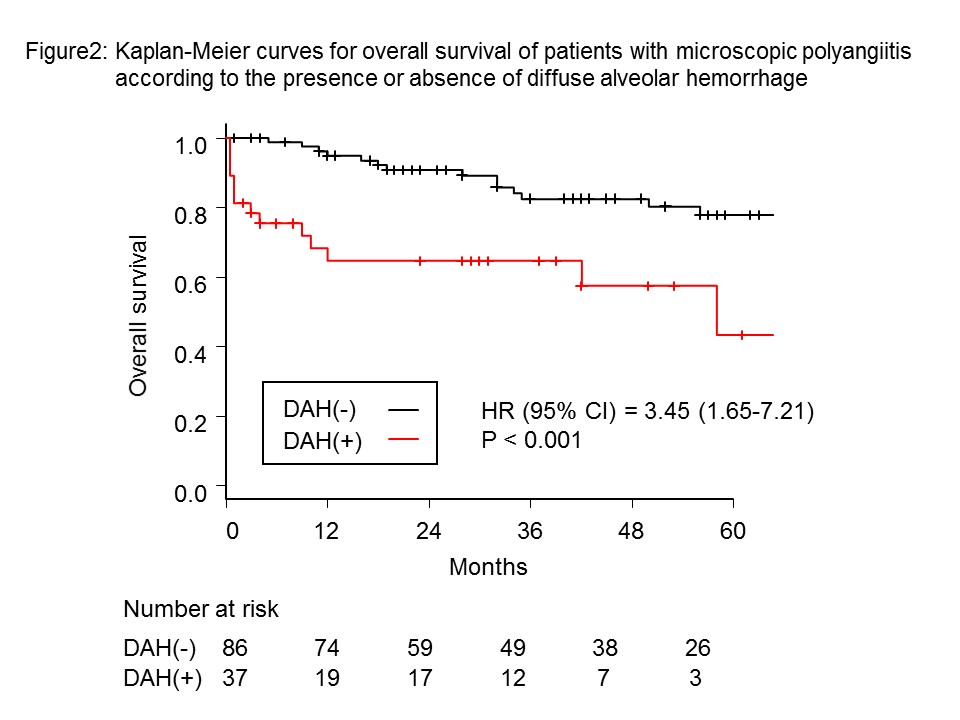
We included 123 consecutive patients with MPO-ANCA positive MPA. DAH was confirmed in 37 (30%) patients, and 33 of them presented DAH at the diagnosis of MPA. In the univariate analyses, airways diseases, absence of ILD, absence of nerve involvement, FFS and BVAS were associated with DAH (Figure 1). In the multivariate analysis, only airways disease (adjusted OR, 3.47; 95% CI, 1.29-9.37) was independently associated with DAH. Airways disease was found in 22 of 37 patients with DAH, and was already pointed out prior to the onset of MPA/DAH in 17 of them. The overall survival rates for patients with DAH were significantly lower than patients without DAH (HR, 3.45; 95% CI, 1.65-7.21) (Figure2).
Conclusion:
DAH frequently occurred in patients with airways disease, and was associated with increased mortality. Airways disease may be involved in the cause of DAH.
To cite this abstract in AMA style:
Kida T, Kaneshita S, Inoue T, Nakabayashi A, Kukida Y, Fujioka K, Nagahara H, Wada M, Seno T, Kohno M, Kawahito Y. Incidence, Predictors, and Outcome of Diffuse Alveolar Hemorrhage in Patients with MPO-ANCA Positive Microscopic Polyangiitis: A Multi-Center Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/incidence-predictors-and-outcome-of-diffuse-alveolar-hemorrhage-in-patients-with-mpo-anca-positive-microscopic-polyangiitis-a-multi-center-retrospective-cohort-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-predictors-and-outcome-of-diffuse-alveolar-hemorrhage-in-patients-with-mpo-anca-positive-microscopic-polyangiitis-a-multi-center-retrospective-cohort-study/