Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Gastrointestinal (GI) involvement is common in patients with systemic sclerosis (SSc), and may lead to malnutrition that adversely affects quality of life, morbidity and mortality. The Global Leadership Initiative on Malnutrition (GLIM) criteria is a new criterion reported to have better sensitivity in detecting malnutrition than the Malnutrition Universal Screening Tool.
Aim: To determine 1) the incidence and prevalence of malnutrition using GLIM criteria 2) the impact of malnutrition on mortality.
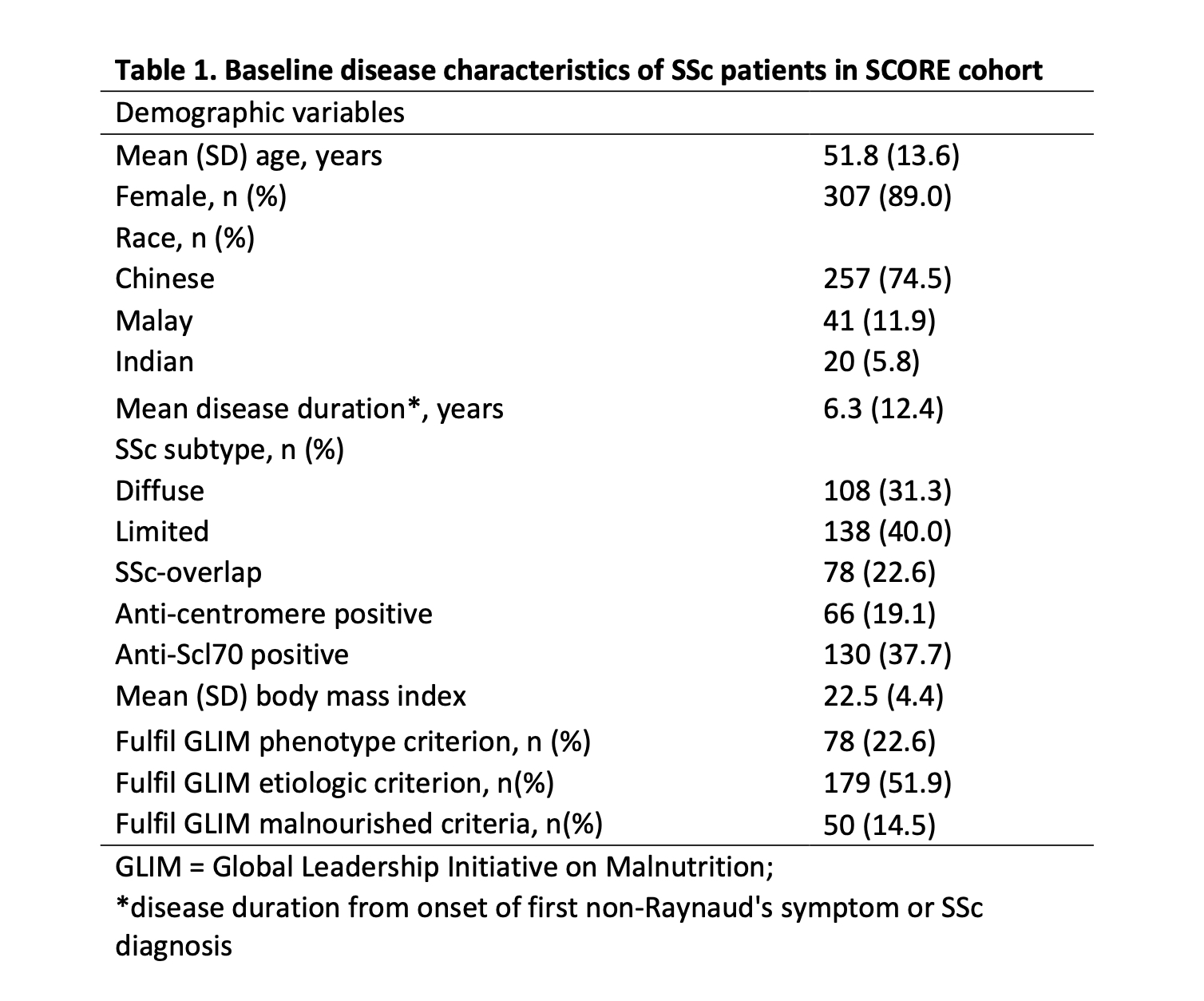
Methods: From 1st of January 2008 to 31st of December 2020, patients fulfilling the SSc ACR/EULAR 2013 criteria were recruited from 3 tertiary rheumatology centres into the Systemic Sclerosis Cohort Singapore (SCORE) cohort. Baseline demographics, disease characteristics, medications and mortality were recorded. Patients with < 6 months followup were excluded from analysis. To fulfil malnutrition with GLIM criteria, at least 1 phenotypic and 1 etiologic criteria are required. For phenotypic criterion, we used BMI < 18.5 (< 70 years old) or BMI < 20 ( >70 years old); for etiologic criterion, we used presence of any one of severe vasculopathy, modified Rodnan skin score > 15, pulmonary hypertension, forced vital capacity < 70%, cardiac involvement, renal crisis, total gastrointestinal tract score > 1.00. Univariate analysis using chi-square test was performed, with p-values < 0.05 considered statistically significant.
Results: Of 345 SSc patients, mean age at baseline visit was 51.8 years, with mean disease duration of 6.3 years. More patients were positive for anti-Scl70 (37.7%) than anti-centromere antibody (19.1%). Mean body mass index was 22.5 (Table 1). Prevalence of malnutrition at baseline visit was 14.5%. Cumulative incidence of malnutrition was 2% at 2 years and 6.4% across the follow-up period (median 47 months). Presence of malnutrition at baseline visit was not associated with mortality, although ever presence of malnutrition during the follow up period was associated with an increased risk of mortality [OR 4.47 (95%CI 3.67-5.26), p-value 0.0008].
Conclusion: This study highlights the burden of malnutrition in SSc patients. Among patients with malnutrition, majority fulfilled GLIM criteria for malnutrition at first visit. The persistence or development of malnutrition throughout the follow-up period was significantly associated with mortality.
References:
1. Santosa A, et al. Lung and Gastrointestinal Complications are Leading Causes of Death in SCORE, a Multi-Ethnic Singapore Systemic Sclerosis Cohort. Scand J Rheumatol 2016; 45:499-506
2. Cederholm T et al. J Cachexia Sarco Muscle 2019;10:207-217
To cite this abstract in AMA style:
Jiang B, Salazar E, Saffari S, Teng G, Lim X, Ng S, Santosa A, Hong C, Low A. Incidence and Prevalence of Malnutrition and Its Impact on Mortality in the Multicentre Singapore Systemic Sclerosis Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/incidence-and-prevalence-of-malnutrition-and-its-impact-on-mortality-in-the-multicentre-singapore-systemic-sclerosis-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-and-prevalence-of-malnutrition-and-its-impact-on-mortality-in-the-multicentre-singapore-systemic-sclerosis-cohort/