Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Pericarditis is the most common cardiac manifestation of systemic lupus erythematosus (SLE). In the general population, pericarditis commonly recurs (~30%), likely due to immune-mediated mechanisms. Given the broad immune dysregulation that drives the pathogenesis of SLE, we sought to identify the frequency and risk factors for the recurrence of pericarditis in this unique population.
Methods: Retrospective cohort study of SLE patients enrolled between 1988 and 2023 at a tertiary medical center. The SELENA revision of the SLE Disease Activity Index was used to define pericarditis, and all follow-up clinical encounters were examined after the first reported episode. Recurrent pericarditis was defined as that occurring at least 6 weeks after the first recorded episode of pericarditis. Statistical significance was defined as a p-value of < 0.05, and a pooled logistic regression was used to estimate odds ratios for risk factors.
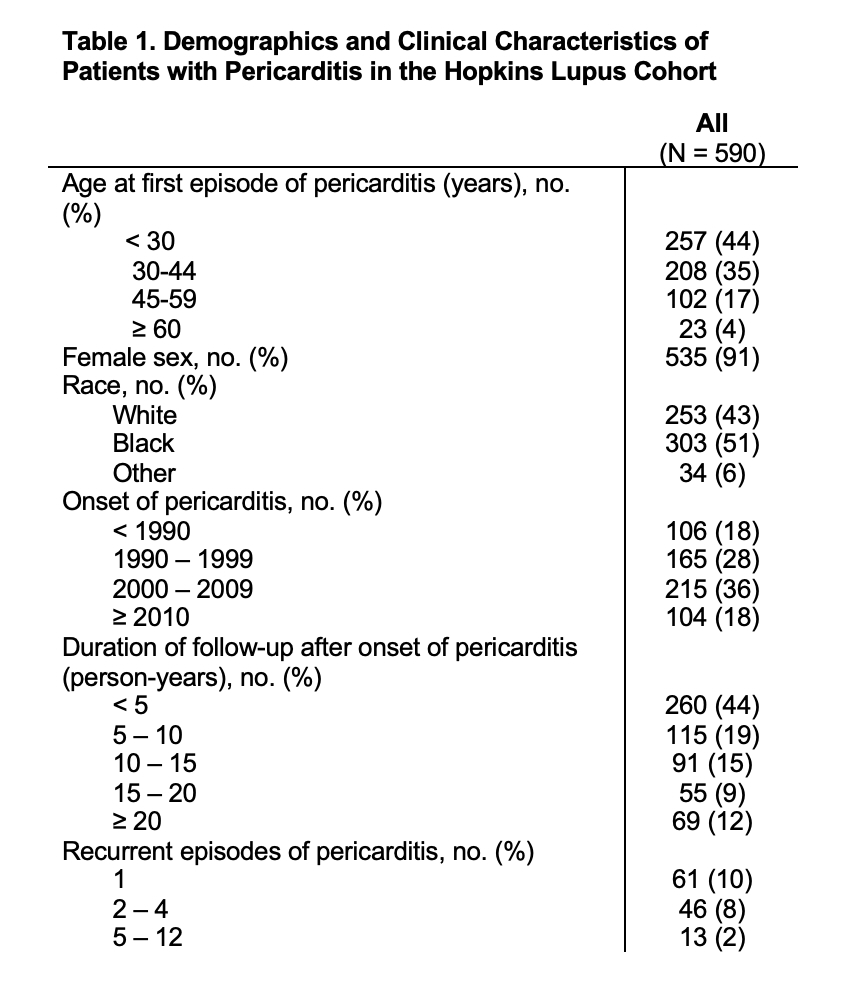
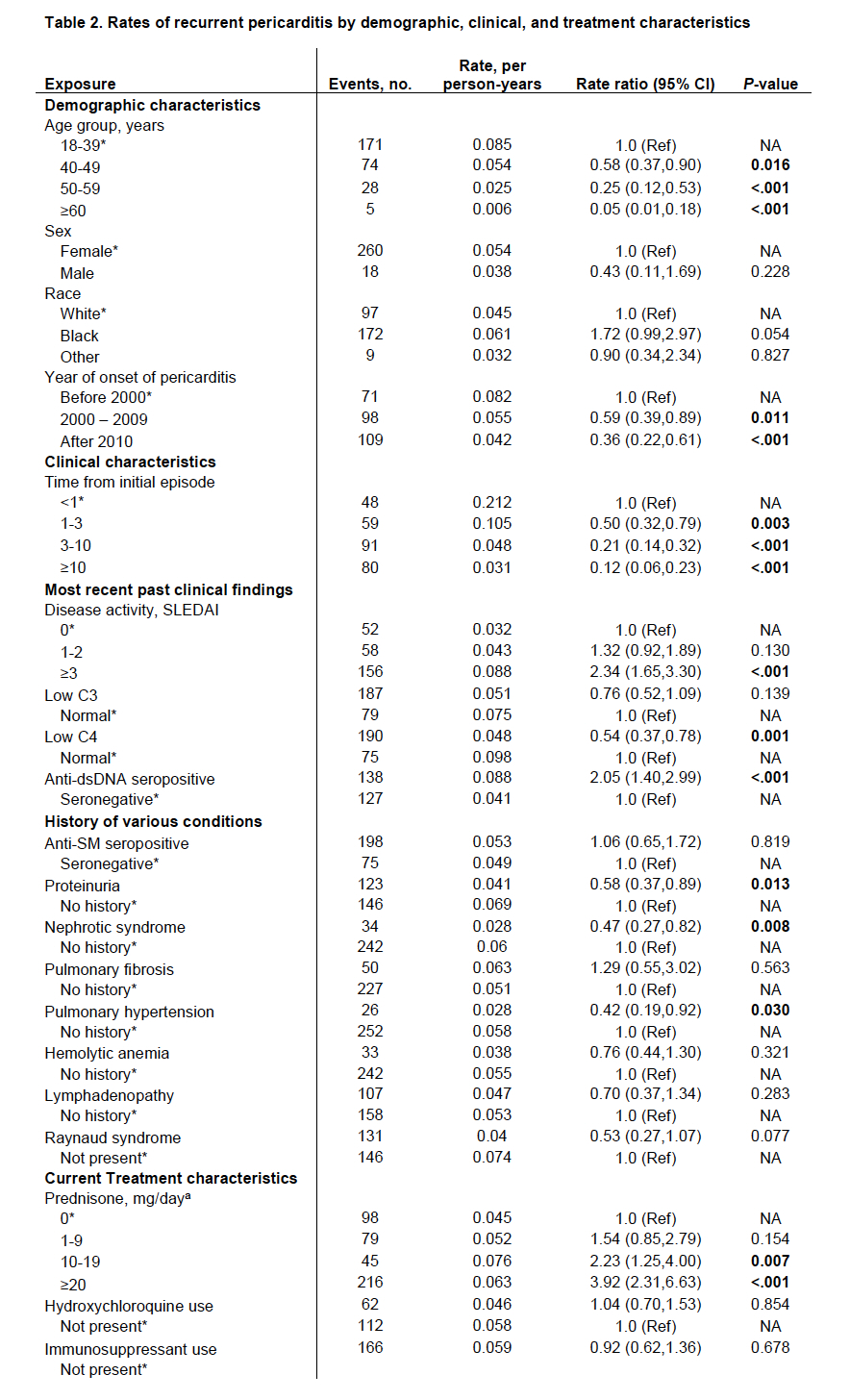
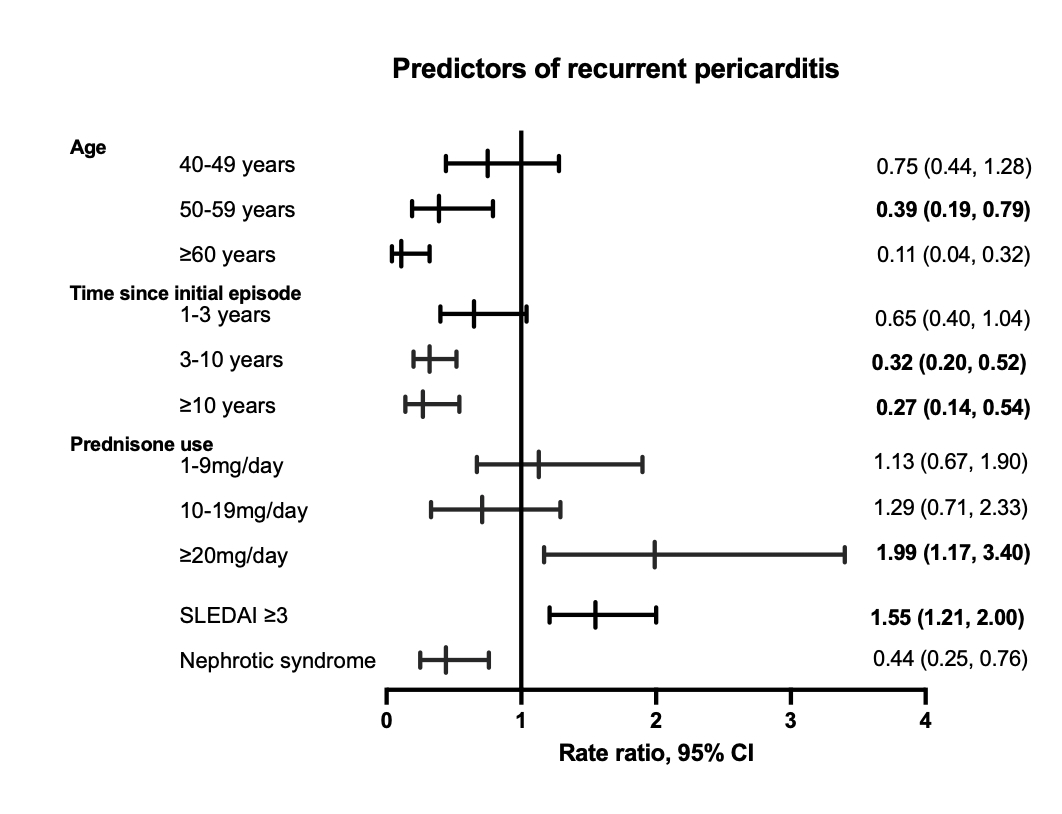
Results: Of 2931 patients in the cohort, 590 patients had a history of pericarditis. During a median follow-up of 7 years (IQR: 3 – 14), 20% (n=120) of patients experienced recurrent pericarditis (Table 1). The majority (51%) experienced only one recurrence, whereas 49% of patients had ≥2 recurrences. Several demographic, clinical, serologic, and treatment characteristics were associated with recurrence in the univariate analysis (Table 2). We performed a multivariate analysis using variables of statistical significance (P < 0.05) and found that independent predictors of recurrence included younger age (≥60 years vs. < 40, RR 0.11 (0.04, 0.32), P < .001), treatment with prednisone ( ≥20 vs. 0 mg, RR 1.99 (1.17, 3.40), P = 0.012), active SLE disease (SLEDAI ≥3 vs. 0, RR 1.55 (1.21, 2.00), P < .001), and time from initial episode (3-10 years vs. < 1, RR 0.32 (0.20, 0.52), P < .001) (Figure 1).
Conclusion: Recurrence of pericarditis in SLE is common (20%) and it is more likely to occur within one year of onset. Younger patients and those with higher lupus activity are at greater risk of recurrence. As in the general population, oral prednisone is independently associated with a higher chance of recurrence in SLE patients, with a dose-dependent effect. These findings set the basis for future studies to define optimal treatment for recurrent pericarditis in SLE patients and indicate that oral corticosteroids should be avoided when treating pericarditis.
To cite this abstract in AMA style:
Kim Y, Lovell J, Diab A, Magder L, Goldman D, Petri M, Adamo L, Fava A. Incidence and Predictors of Recurrent Pericarditis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/incidence-and-predictors-of-recurrent-pericarditis-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-and-predictors-of-recurrent-pericarditis-in-systemic-lupus-erythematosus/