Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with SLE can experience a variety of neuropsychiatric manifestations across 19 recognized syndromes (1999 ACR Nomenclature). Studies of neuropsychiatric SLE (NPSLE) have been primarily from academic center cohorts. The purpose of this study was to determine the incidence and predictors of NPSLE using a large population cohort.
Methods: We utilized TriNetX, an electronic health record database including 46 health care organizations, representing community hospitals and academic medical centers across the United States. We identified patients with incident SLE (defined as ≥ 2 ICD codes >30 days and < 2 years apart, with ≥2 years enrollment prior to the first SLE code). Within this cohort, we identified all NPSLE events, identified by ICD codes corresponding with each of the 19 syndromes occurring within 2 years before or following the first SLE code, regardless of attribution to SLE. We assessed the incidence of NPSLE overall, according to central vs. peripheral nervous system syndromes, and within categories of potentially inflammatory neurologic syndromes, psychiatric, cerebrovascular (CVA), and seizures. We identified patients with early NPSLE, with ≥1 syndrome within one year of SLE onset, and assessed their characteristics. We assessed patient factors associated with each category of NPSLE using logistic regression, including age at SLE onset, sex, race and ethnicity, diagnosis of antiphospholipid syndrome (APS) or Sjogren’s syndrome, and early hydroxychloroquine (HCQ) use, assessed within two years prior to the first SLE diagnosis code and subsequent 12 months.
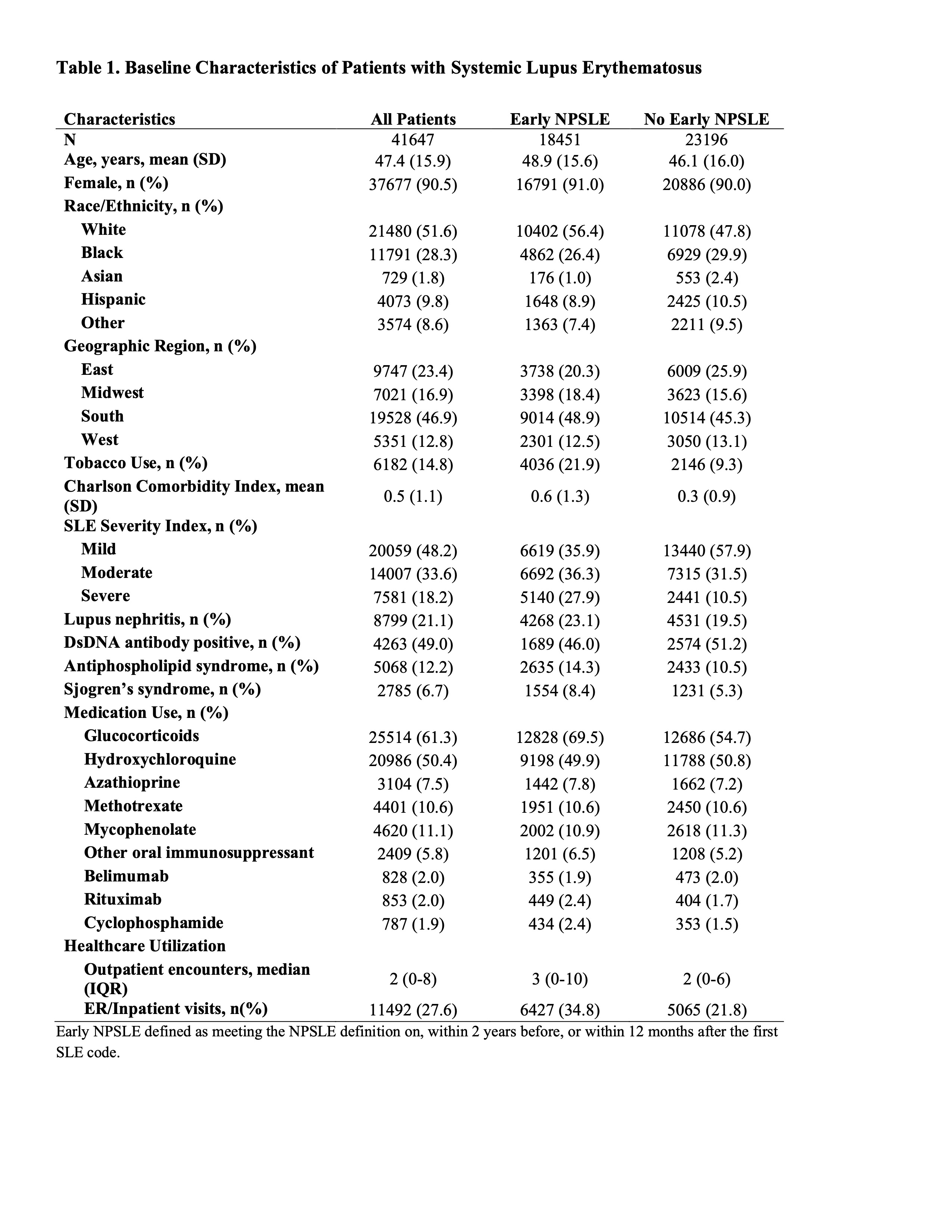
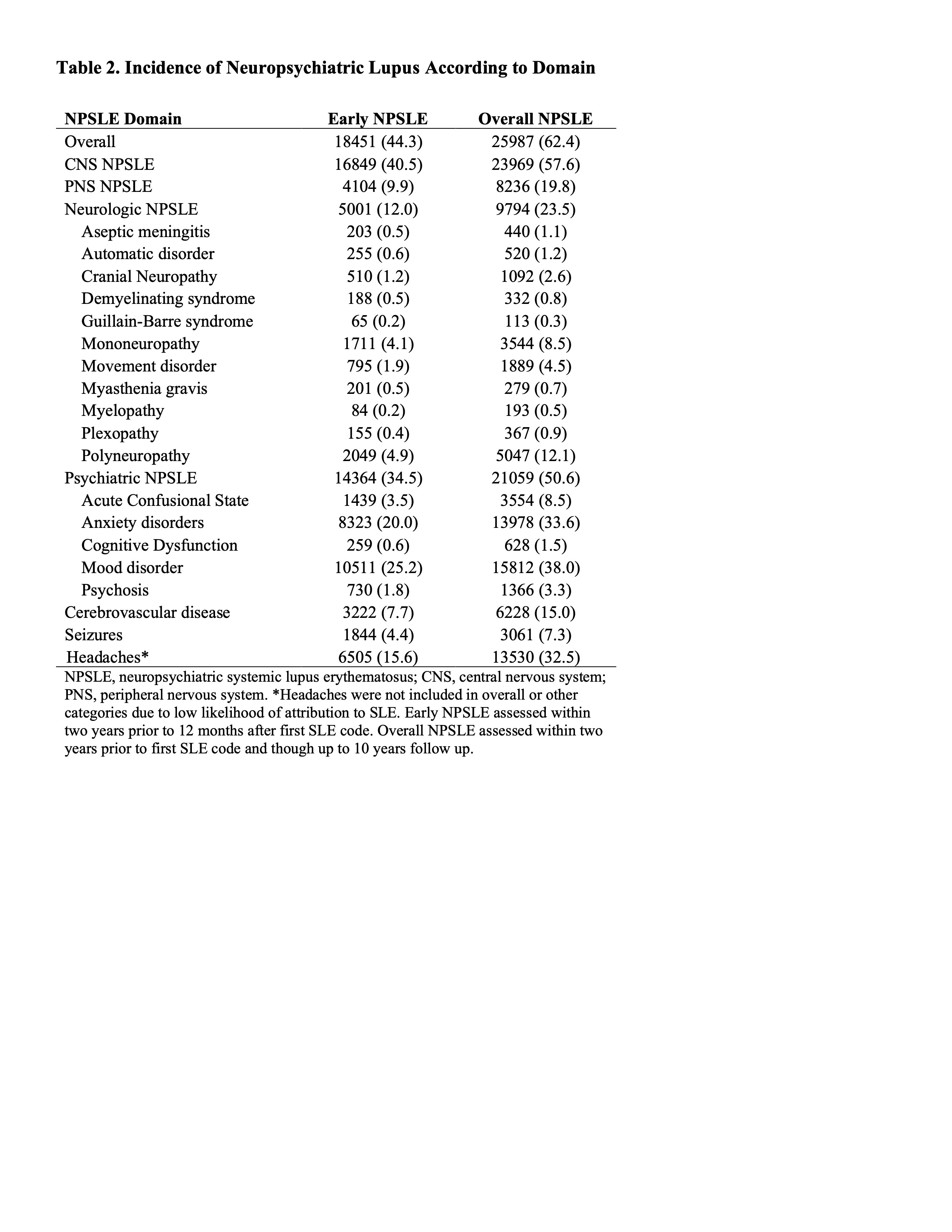
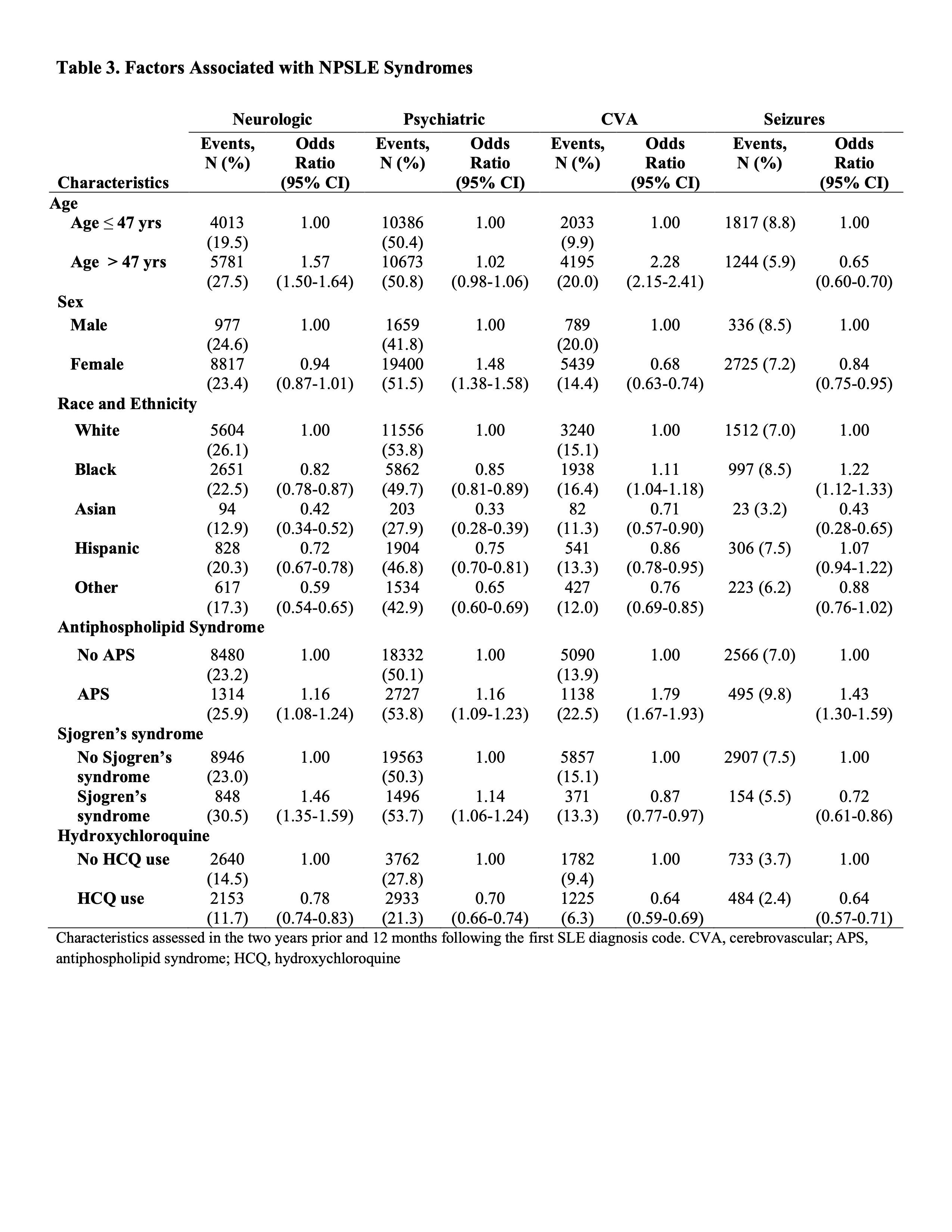
Results: We identified 41,647 patients with incident SLE. The mean age was 47.4 years; 52% were non-Hispanic White and 28% were Black (Table 1). From this cohort, 18,451 (44%) had early NPSLE, and 63% developed NPSLE over mean 4.4 years follow-up after SLE onset. Psychiatric NPSLE, including mood disorders and anxiety disorders, were the most common NPSLE manifestations (Table 2). 12% had early neurologic NPSLE, rising to 24% overall, followed by CVA and seizures in frequency. Patients with ≥ 1early NPSLE event were more likely to be White (56% vs. 48% without early NPSLE) and use tobacco (22% vs 9%). For specific NPSLE categories, older age was associated with higher odds of neurologic NPSLE and CVA but lower odds of seizures (Table 3). Females had higher odds of psychiatric NPSLE. Black patients had higher odds of seizures and CVA, but Black, Asian, and Hispanic race and ethnicity had lower odds of neurologic and psychiatric syndromes than in White patients with SLE. APS was associated with all categories of NPSLE, and Sjogren’s syndrome was associated with neurologic and psychiatric NPSLE. Baseline HCQ use was associated with a lower odds of all NPSLE categories.
Conclusion: In this large EHR-based inception cohort of patients with SLE, we identified a high burden of NPSLE events both early in the disease course and increasing over time. We also identified different predictors for different categories of NPSLE, suggesting heterogeneity in these syndromes. APS was associated with all types of NPSLE, while HCQ use may be protective. Limitations include the challenge of attributing NPSLE and possibility of misclassification.
To cite this abstract in AMA style:
Silva Y, Zhou B, Lee G, Panchot K, Choi H, Jorge A. Incidence and Predictors of Neuropsychiatric Lupus—a Contemporary Cohort Study Across the United States [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/incidence-and-predictors-of-neuropsychiatric-lupus-a-contemporary-cohort-study-across-the-united-states/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-and-predictors-of-neuropsychiatric-lupus-a-contemporary-cohort-study-across-the-united-states/