Session Information
Date: Saturday, November 7, 2020
Title: Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The purpose of this analysis was to assess the frequency of inadequate response (IR) over 1 year associated with advanced therapy (AT) initiation among psoriatic arthritis (PsA) patients in the US using a claims-based algorithm that was originally developed and validated for rheumatoid arthritis1. Baseline factors associated with IR to AT were also analyzed.
Methods: This was a retrospective cohort study using claims data from the HealthCore Integrated Research Database®. Adult patients with PsA who initiated an AT (TNFi: adalimumab, certolizumab, etanercept, golimumab, infliximab; non-TNFi biologic: abatacept, ixekizumab, secukinumab, ustekinumab; other: apremilast, tofacitinib) from 7/1/2016 to 8/31/2018 and had continuous enrollment ≥6 months before and ≥12 months after index date (date of first biologic claim) were included. The index AT was defined as the first AT prescribed during the study time period. Patients were identified as having IR to their index AT if during the 12 months after index date (defined as date of first AT claim) they had one or more of the following: low adherence (defined as proportion of days covered (PDC)< 80%), switched/added a new AT, added a new conventional synthetic immunomodulator (e.g. methotrexate), increased dose/frequency of AT, had >1 glucocorticoid injection/infusion, addition or dose increase of oral glucocorticoids, used a new topical treatment, actinotherapy, or retinoids, or used a new pain medication. Baseline characteristics were compared between responders and IRs using Chi-squared tests for categorical variables and t-tests for continuous variables. A multivariable logistic regression model was constructed to identify baseline characteristics associated with IR to index AT.
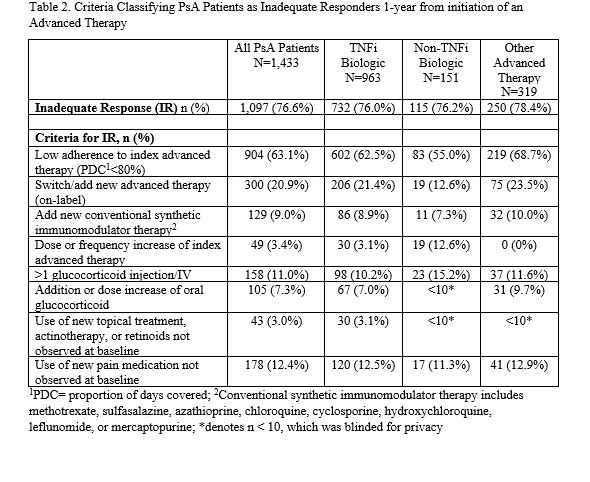
Results: A total of 1,433 PsA patients were included in this analysis. Mean age was 49 years, 47% were male, 67% initiated a TNFi, 22% initiated other ATs, and 11% initiated a non-TNFi biologic (Table 1). Over the 1-year follow-up period, 77% of PsA patients had IR to their index AT: 63% of patients had low adherence, 21% switched/added a new AT, 9% added a new conventional synthetic immunomodulator, 3% had a dose/frequency increase of their index AT, 11% had >1 glucocorticoid injection/infusion, 7% had an addition/dose increase of oral glucocorticoids, 3% used a new topical treatment, actinotherapy or retinoids, and 12% used a new pain medication (Table 2). Inadequate responders were more likely to be female (odds ratio (OR)=1.37; p=0.017), have anxiety or depression (OR=1.80; p=0.002), and have a higher baseline Quan-Charlson Comorbidity Index (QCI) score (OR=1.21; p=0.036); while patients with baseline use of methotrexate were more likely to be responders (OR=0.72; p=0.015) (Table 3). Prior exposure to TNFi was associated with a 2.14-fold greater odds of non-response (p=0.003).
Conclusion: Over 75% of PsA patients had an IR to their index AT 1 year after initiation, mostly driven by low adherence and switching to or adding on a new treatment. Health plan claims data appears useful to classify inadequate responders in PsA, and additional research should be done to further validate this claims-based algorithm in a clinical setting.
To cite this abstract in AMA style:
Birt J, Grabner M, Isenberg K, Hunter T, Teng C, Shan M, Lisse J, Wu J, Griffing K, Curtis J. Inadequate Response Among Psoriatic Arthritis Patients Prescribed Advanced Therapy in a Real-world US Commercially Insured Population [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/inadequate-response-among-psoriatic-arthritis-patients-prescribed-advanced-therapy-in-a-real-world-us-commercially-insured-population/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inadequate-response-among-psoriatic-arthritis-patients-prescribed-advanced-therapy-in-a-real-world-us-commercially-insured-population/