Session Information
Date: Sunday, November 12, 2023
Title: (0229–0251) Metabolic & Crystal Arthropathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with gout are at increased risk of acute myocardial infarction (AMI). However, the clinical course, secondary prophylaxis and mortality after AMI has not been previously studied. The aim of this study is to investigate the in-hospital treatment, secondary prevention, and all-cause and cardiovascular disease (CVD)-related mortality after the first-ever AMI in patients with gout compared to the general population.
Methods: Using data from regional and national population-based registers, we identified all patients in Western Sweden with a diagnosis of gout at both primary and specialty care and a first-ever AMI in the period 2006-2016. Up to five individually matched controls with a first-ever AMI (matched on sex and admission year) were identified as comparators. Follow-up started at the date of admission for the first-ever AMI and ended at death, emigration, or 365 days of follow-up after the AMI, whichever occurred first. The in-hospital treatment and secondary prevention in gout cases and controls were compared by using logistic regression analysis with adjustments for age. Cox regression analysis was used to assess the 1-year mortality with adjustments for age, baseline comorbidities, and medication within 6 months before the start of follow-up.
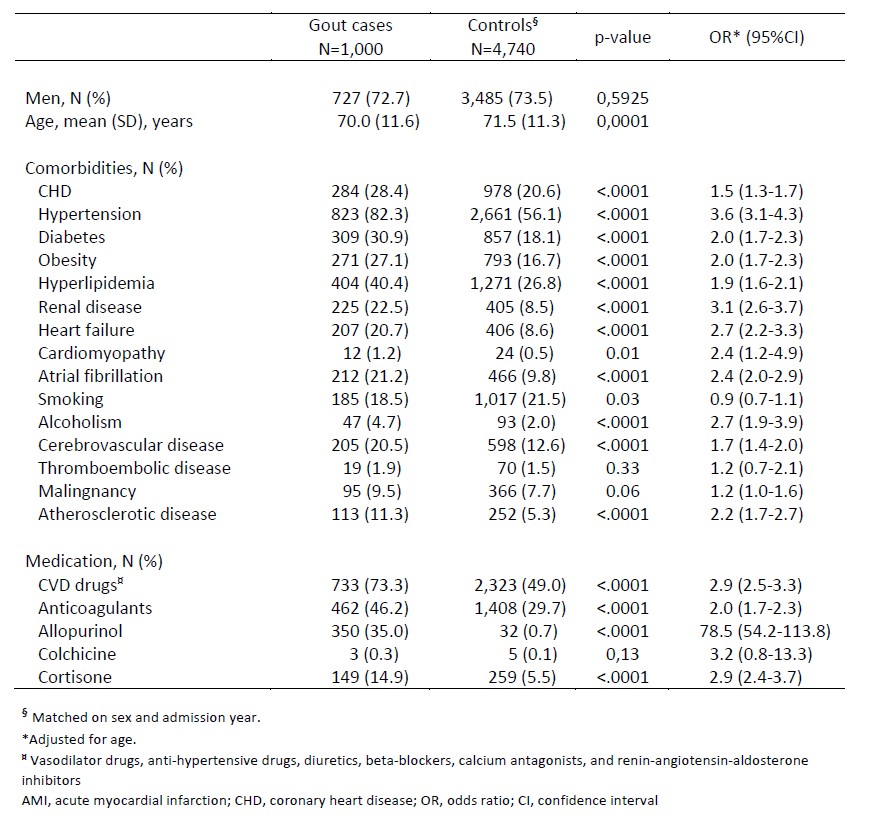
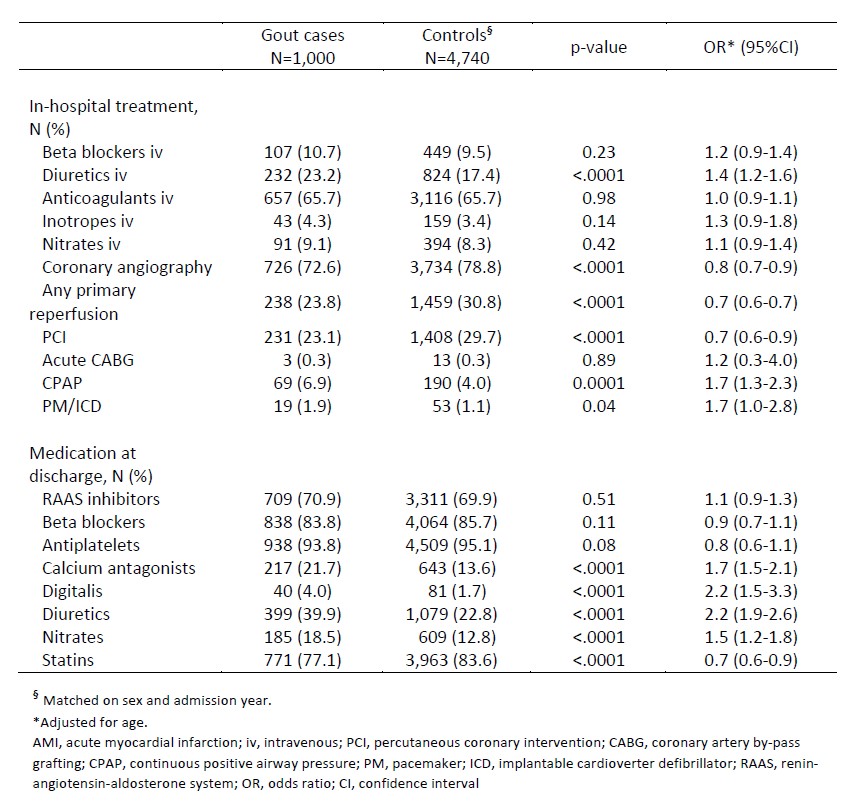
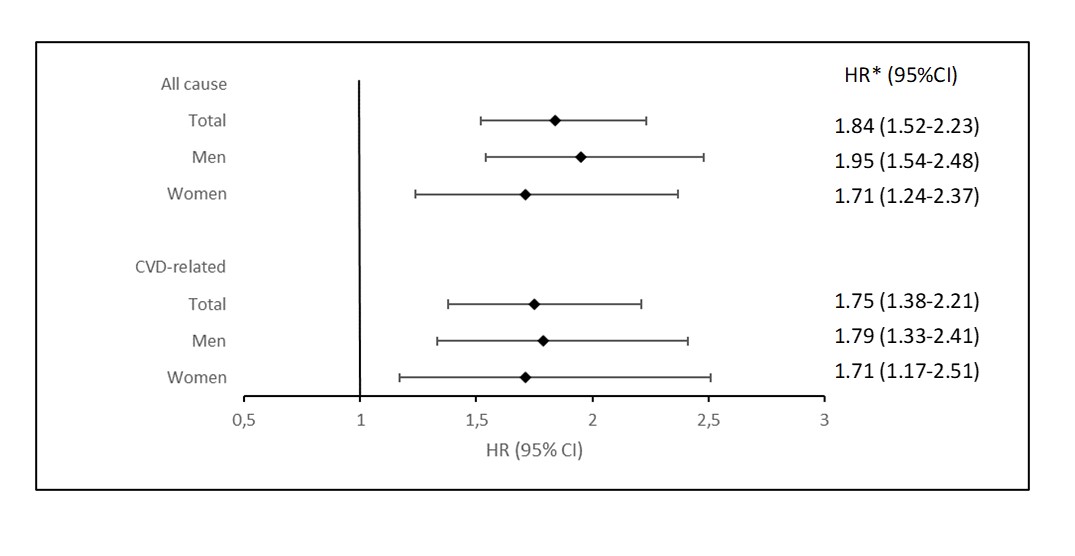
Results: We identified 1,000 patients with gout and a first-ever AMI (men, 72.7%; mean age, 70.0 years) and 4,740 matched general population comparators (men, 73.5%; mean age, 71.5 years). At admission, patients with gout hade significantly more comorbidities (Table 1). The in-hospital treatment differed significantly between cases and controls. Patients with gout were more likely to receive treatment with diuretics and continuous positive airway pressure (CPAP), and less likely to undergo coronary angiography, percutaneous coronary intervention (PCI), or any primary reperfusion (Table 2). At discharge, patients with gout were less often prescribed statins, and more often prescribed nitrates, diuretics, digitalis, and calcium antagonists (Table 2). The prescription of antiplatelets, renin-angiotensin-aldosterone inhibitors, or beta-blockers did not differ significantly between cases and controls (Table 2). The 1-year all-cause and CVD-related mortality was significantly higher in gout patients as compared to the general population (HR, 1.84; 95%CI, 1.52-2.23; and HR, 1.75; 95%CI, 1.38-2.21, respectively) (Figure 1).
Conclusion: Patients with gout were less likely to undergo coronary angiography and PCI during hospitalization for the first-ever AMI and were less likely to be prescribed statins at discharge compared to the general population. The all-cause and CVD-related mortality was significantly higher in patients with gout which might be partly related to differences in in-hospital treatment and secondary prevention.
*Adjusted for age, baseline comorbidities, and medication within 6 months before the start of follow-up.
HR, hazard ratio; CI, confidence interval; CVD, cardiovascular disease
To cite this abstract in AMA style:
Drivelegka P, Jacobsson L, Zverkova-Sandström T, Dehlin M. In-hospital Treatment, Secondary Prevention, and Mortality After First-ever Acute Myocardial Infarction in Patients with Gout [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/in-hospital-treatment-secondary-prevention-and-mortality-after-first-ever-acute-myocardial-infarction-in-patients-with-gout/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-hospital-treatment-secondary-prevention-and-mortality-after-first-ever-acute-myocardial-infarction-in-patients-with-gout/