Session Information
Date: Monday, November 8, 2021
Title: Health Services Research Poster II: Care Models and Innovation (1061–1082)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: In many health care jurisdictions the demand for rheumatology consultation exceeds the capacity to provide timely access for all referrals. This has highlighted the importance of enhanced triage to ensure timely access to care for those with the most urgent need. The purpose of this project was to design and evaluate a systematic centralized triage system to improve identification of patients with new onset inflammatory arthritis.
Methods: In this prospective randomized study, half of new referrals received for arthritis at a single academic health care centre with 10 attending staff rheumatologists were assigned to the “enhanced” centralized triage process (intervention); the other 50% of referrals were assessed using the “standard” current triage system (control). Referrals were randomly assigned to a triage arm using a randomization schedule generated through REDCap. In the intervention arm, referrals were triaged based on the probability of inflammatory arthritis using a combination of laboratory data including rheumatoid factor, anti-cyclic citrullinated peptide antibodies, C-reactive protein twice the upper limit of normal and a scoring algorithm using a validated early inflammatory arthritis questionnaire. Referrals in the control arm were triaged by individual rheumatologists as per their usual practice. Data regarding referral content, patient demographics, diagnosis, triage category, disease activity and time from receipt of referral to first assessment were collected and entered into a REDCap database.
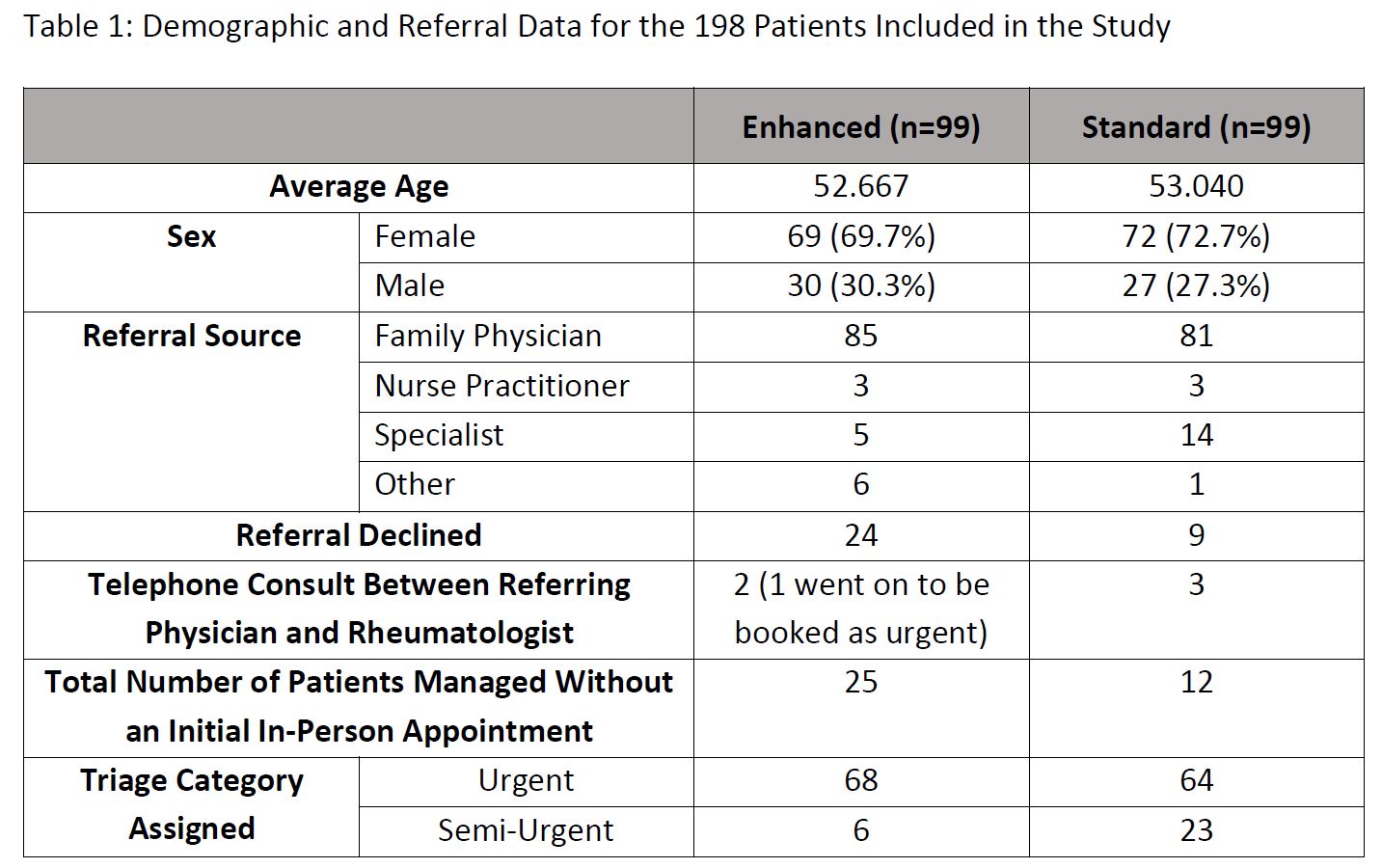
Results: 198 patients were included in the study, 99 patients in each arm (Table 1). A higher percentage of patients requiring urgent assessment were confirmed to have inflammatory arthritis in the intervention arm compared to the control arm (54.4% vs .46.9%) although this did not reach statistical significance (P = 0.384). More patients in the intervention arm compared to the control arm (25 vs 12; P = 0.018) were managed without requiring an in-person clinic appointment, in which case initial treatment recommendations were sent directly to the referring physician. This reduced in person clinic visits and avoided prolonged delays in treatment implementation. In addition, wait times for rheumatology assessment for those with inflammatory arthritis was 17 days shorter in the intervention arm (70.2 vs. 87 days) although this did not reach statistical significance (P = 0.191).
Conclusion: For patients referred for suspected inflammatory arthritis, a systematic centralized triage system may lead to improved outcomes; these include better agreement between triage suspected diagnosis and rheumatologist confirmed diagnosis of inflammatory arthritis, improved wait times and more referrals managed without an unnecessary rheumatology assessment.
To cite this abstract in AMA style:
Roche K, Hanly J, MacKinnon J, Parlee S, Taylor T, Bakowsky V, Gunn C, Harris N, Roberts J. Improving Rheumatology Resource Utilization and Access to Specialty Care for Patients with Early Inflammatory Arthritis Through Enhanced Triage [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/improving-rheumatology-resource-utilization-and-access-to-specialty-care-for-patients-with-early-inflammatory-arthritis-through-enhanced-triage/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-rheumatology-resource-utilization-and-access-to-specialty-care-for-patients-with-early-inflammatory-arthritis-through-enhanced-triage/