Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatic diseases are at increased risk of invasive pneumococcal disease. Both pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) are recommended for patients on immunosuppressant medications. However, under-vaccination of this population is common. The aim of this quality improvement project was to decrease the percent of patients in Tennessee Valley Healthcare System (TVHS) Rheumatology clinic due for vaccination in a given month from the baseline of 36% to a goal of 28% within 6 months.
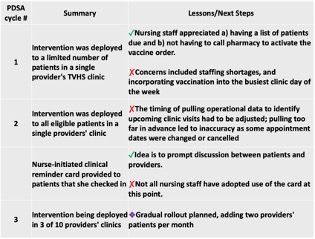
Methods: Barriers to vaccination were identified and an intervention was designed incorporating patient outreach, provider outreach, and health system components (Figure 1). The primary outcome measure was the percent of randomly sampled patients due for a pneumococcal vaccination, assessed monthly. Process measures include the number of vaccinations administered in rheumatology clinic each month. Balancing measures included qualitative feedback from staff. The Plan Do Study Act (PDSA) cycle methodology was used to test and analyze process changes (Figure 2).
Results: Statistical process control (SPC) charts were used to visualize results (Figure 3). Post-implementation, the overall percent of patients due for a pneumococcal vaccination is statistically unchanged thus far, though trending downwards. The number of pneumococcal vaccines administered in clinic was steadily rising with a special cause signal seen in January 2020, however this change was not sustained. In the 9 month pre-intervention period, 38 vaccinations in total were administered in Rheumatology clinic, whereas in the post-intervention implementation period 54 vaccines were given in just 5 months.
Conclusion: A combination of operational data use, pre-visit planning, and patient outreach can lead to increased pneumococcal vaccination rates in a rheumatology clinic setting. The lack of statistically significant change in our primary outcome measure is likely explained by our sampling strategy, which samples from all providers’ clinics, though the intervention had only been rolled out in about half of the providers’ clinics before the COVID-19 pandemic. A more upstream process measure is the number of pneumococcal vaccinations administered in clinic each month, where we have seen signs of improvement. Next steps include 1) ongoing rollout to the clinics of all rheumatology providers, 2) development of an educational intervention for providers regarding the complex pneumococcal vaccination schedule, and 3) adaptations to the clinic templated note to include reminders and facilitate ordering.
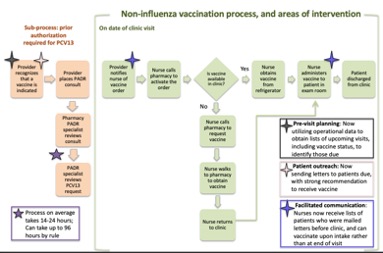 Figure 1: Process Map and Intervention
Figure 1: Process Map and Intervention
To cite this abstract in AMA style:
Homann S, Ormseth M, Roumie C, Dittus R. Improving Pneumococcal Vaccination in Veterans with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/improving-pneumococcal-vaccination-in-veterans-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-pneumococcal-vaccination-in-veterans-with-rheumatic-diseases/