Session Information
Date: Sunday, November 13, 2022
Title: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Osteoporosis, including the clinical event of fragility fracture is an ever-increasing public health burden. Effective screening techniques and well as therapies to reduce future fracture risk are well defined and readily available. The US Preventative Services Task Force recommends screening for osteoporosis in all women age 65 and over. However, it has been well described that screening rates, especially in non-white compared to white populations are low. The aim of this work is to improve the screening rates for osteoporosis through dual-energy x-ray absorptiometry (DXA), focusing on non-white individuals across a single academic health system.
Methods: Within a single academic health system, two specific interventions were implemented starting in the summer/fall of 2021 to increase the rates of osteoporosis screening in women age 65 and over with a specific target of increasing osteoporosis screening in non-white populations by 4% by the end of the time period October 2021 – September 2022. First, system-wide, a Care Gap was implemented in the electronic health record to notify PCPs at the time of a patient visit that an individual did not have a DXA result within the electronic health record. Second, specific primary care practices with the highest rates of non-white women age 65 and over without a recorded DXA were targeted and received individualized lists of their patients without osteoporosis screening and with institutional support, a care pathway was developed to then directly contact, counsel and then if agreeable arrange for DXA screening. Cumulative screening rates in the target population were calculated monthly from the time of implementation.
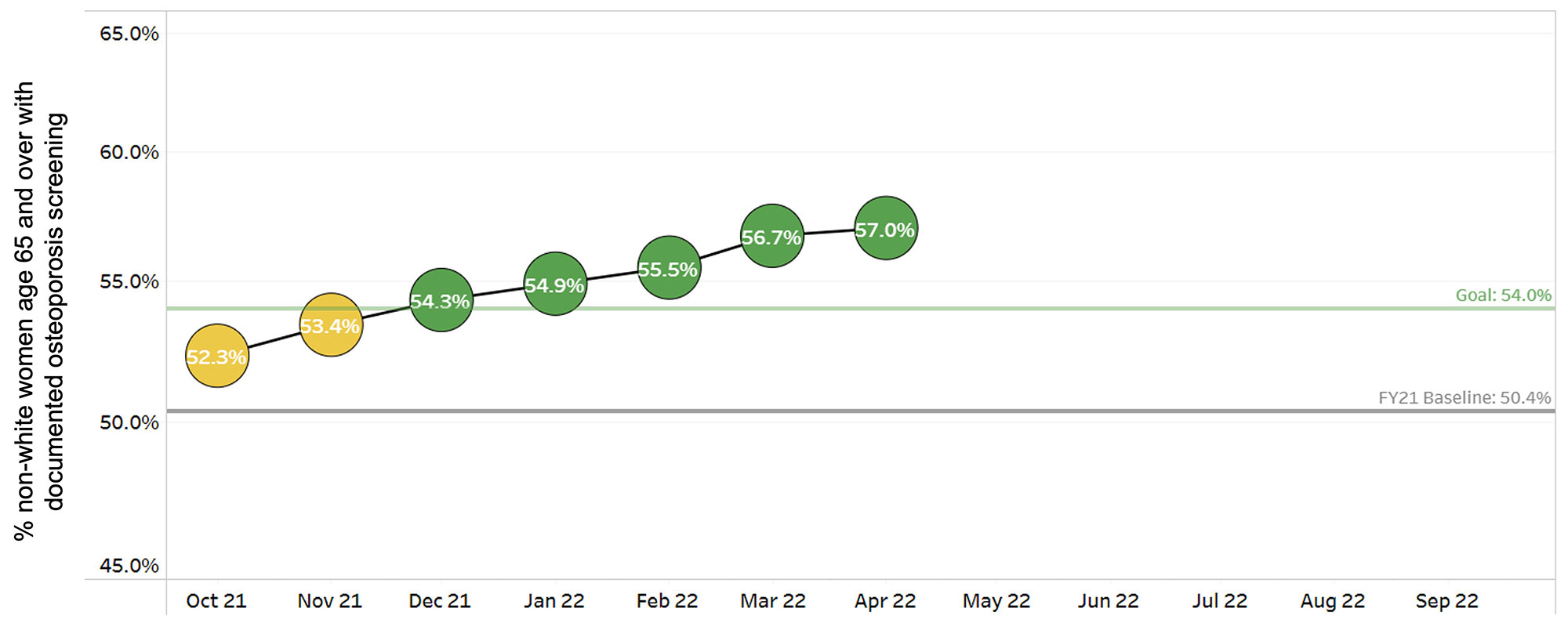
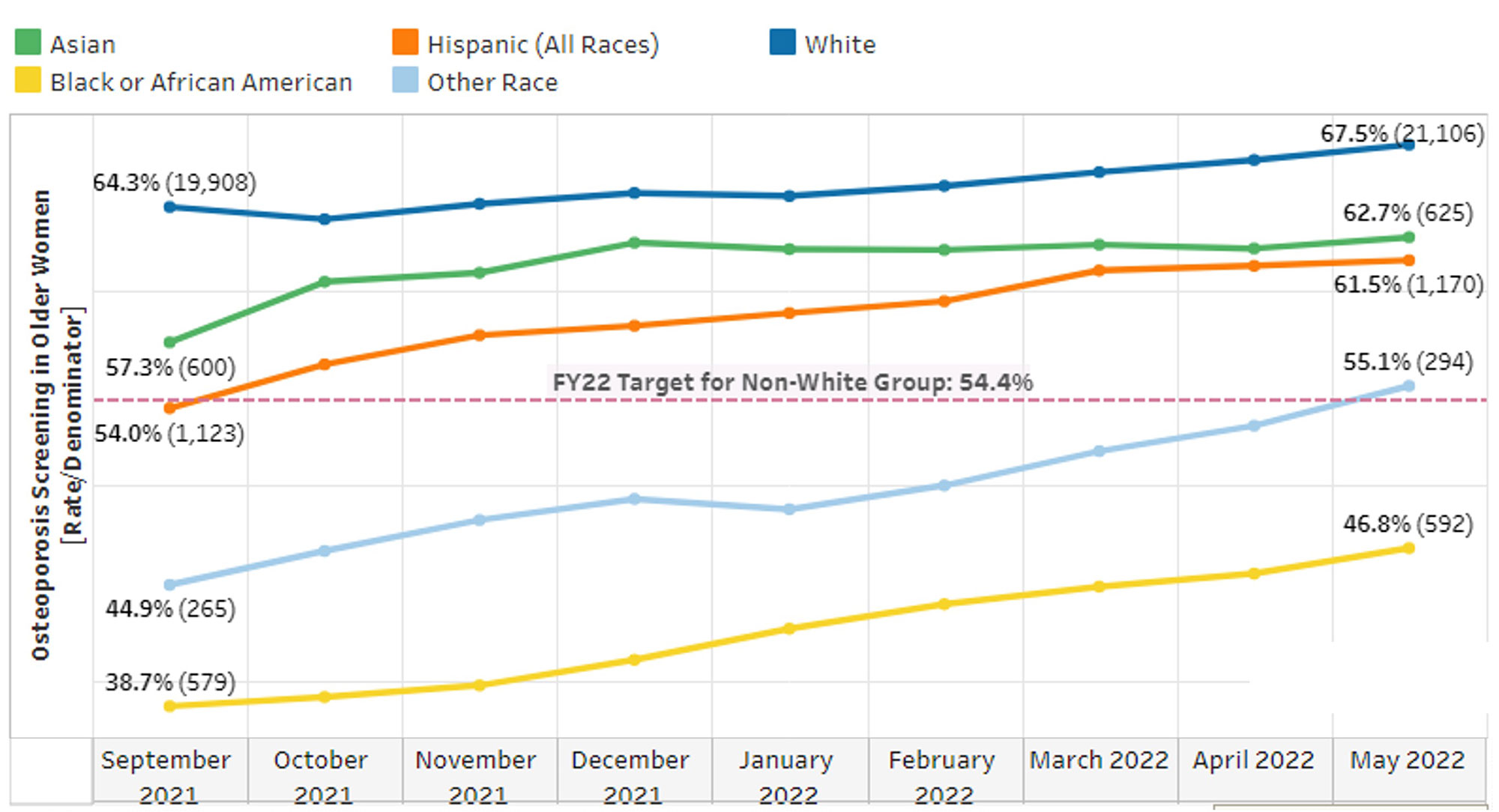
Results: At baseline (October 2020 – September 2021), 50.4% of non-white women age 65 and over had received DXA testing, compared to 64.3% of white women. With the implementation of the Care Gap in July 2021 and targeted interventions within 10 Primary Care Practices starting in September 2021, total screening rates in non-white individuals has improved month by month to a current documented screening rate of 57% (Figure 1), exceeding the initial target goal of the initiative. While screening in all racial groups have improved over time, Black or African-American individuals continue to have much lower overall screening rates (46.8%), compared to their white (67.5%), Asian (62.7%) and Hispanic (61.5%) counterparts (Figure 2).
Conclusion: Using both general and specific interventions to target underrepresented populations is able to improve screening rates for osteoporosis. Additional work will focus on eliminating racial inequalities with screening as well as ensuring that those who are screen positive are linked into osteoporosis care.
To cite this abstract in AMA style:
Brochu M, Marcus K, Latorre S, Wanjau F, Garg A, Alper E, Lyu R, Wilkie T, Cheah J. Improving Osteoporosis Screening in Individuals of Color [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/improving-osteoporosis-screening-in-individuals-of-color/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-osteoporosis-screening-in-individuals-of-color/