Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Smoking is prevalent among patients with spondyloarthropathies (SpA) and is associated with higher disease activity, poorer quality of life, and dampened response to biologic therapy. Despite the strong recommendation for smoking cessation in the 2018 American College of Rheumatology guidelines for management of psoriatic arthritis, providers do not routinely counsel smokers in the context of their disease (SpA). The goal of this quality improvement project was to improve documentation of smoking cessation counseling for SpA smokers at a busy Veteran Affairs (VA) Medical Center rheumatology clinic. The VA is an ideal setting to conduct this project since robust, evidence-based tobacco cessation modalities can be integrated into primary and specialty clinic care settings.
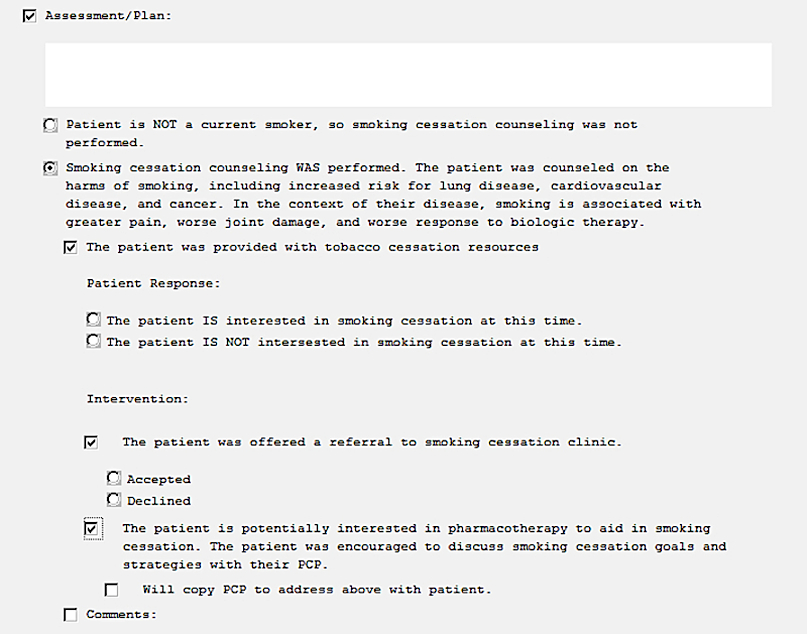
Methods: Baseline documentation rates of smoking status and smoking cessation counseling were obtained via chart review of patients diagnosed with ankylosing spondylitis, inflammatory bowel disease (IBD)-associated arthritis, and psoriatic arthritis who were current smokers seen for follow-up (8/2017-6/2018). We implemented a four step multi-modal intervention that included: a) a modified clinic note template (effective 1/2020) with specific prompts to address tobacco use (Figure 1), b) educating providers and nurses regarding the importance of counseling and template adherence, c) introducing a paper slip on top of intake documents to remind providers to inquire about smoking, and d) equipping the clinic with brochures on cessation resources. Preliminary post-intervention data from follow-up visits were collected until the novel coronavirus disease 2019 (COVID-19) outbreak altered clinic workflow (1/2020-3/2020). Differences in documentation rates pre- and post-intervention were analyzed using Fischer’s exact test.
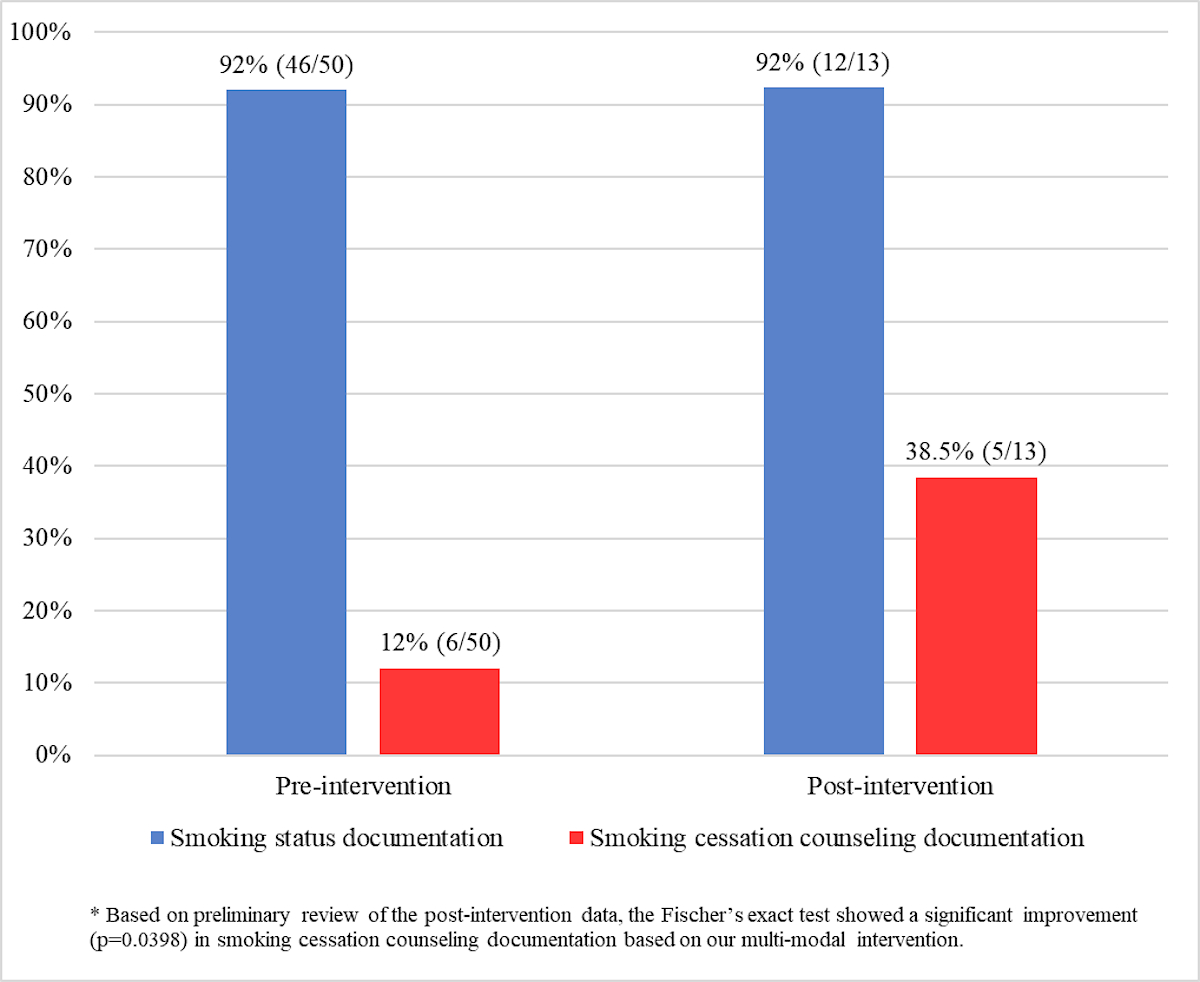
Results: In the pre-intervention phase, 50 smokers were identified among 498 SpA patients, indicating a 10% baseline smoking rate. Rheumatologists documented smoking status for 92% of smokers and smoking cessation counseling for 12% of smokers. In the early post-intervention phase, we identified 13 smokers (15%) among 87 SpA patients. Utilization of the modified clinic note template was 30% (26/87). With our multi-modal intervention, the smoking status documentation rate remained at 92%, while the counseling documentation rate increased to 38.5% (Figure 2).
Conclusion: The baseline documentation rate of smoking cessation counseling for SpA smokers is low among rheumatology providers. Because of the COVID-19 outbreak, reduced outpatient volumes and unanticipated changes in clinic workflow have imposed limitations on post-intervention data collection. Nevertheless, our preliminary data suggest that a multi-modal intervention can improve documentation of smoking cessation counseling; this improvement may be sustainable with continued staff education on counseling and consistent template use. Our next steps will involve evaluation of receipt of smoking counseling and further reduction in smoking rates.
To cite this abstract in AMA style:
Chao Y, Hutto J, Joerns E, Arora R, Makris U, Reddy S. Improving Documentation of Smoking Cessation Counseling Among Spondyloarthropathy Smokers [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/improving-documentation-of-smoking-cessation-counseling-among-spondyloarthropathy-smokers/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-documentation-of-smoking-cessation-counseling-among-spondyloarthropathy-smokers/