Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Treat-to-target is a guiding principle in the management of rheumatoid arthritis (RA), and randomized clinical trials demonstrate its value in improving outcomes. However, implementation remains infrequent and standardized methods for establishing individual treatment targets remain problematic and lack input from patients. Building on a collaboration between a non-profit organization and an academic rheumatology center, we aimed to gain greater understanding of patient treatment goals and preferences and examine how these may relate to treatment satisfaction or success.
Methods: A 28-item anonymous, web-based questionnaire developed and pilot-tested by the study team was presented over 7 days in 2019 on a secure survey system preventing multiple entries. Eligible participants were U.S. residents age ≥18 years with a self-reported diagnosis of RA by a medical professional. Participants were recruited through email, social media, and the web. Participants were asked closed- and open-ended questions about socio-demographics, their RA disease activity (DA), diagnosis and DMARD history, improvement from RA treatment, and the nature of RA treatment goals or plans created with their provider. Analyses included descriptive statistics with chi-square and rank sum tests for comparisons.
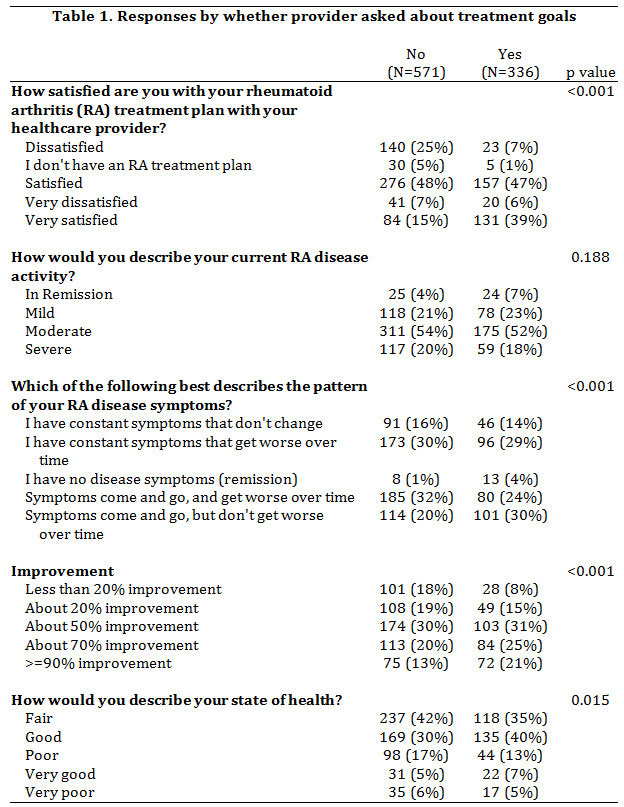
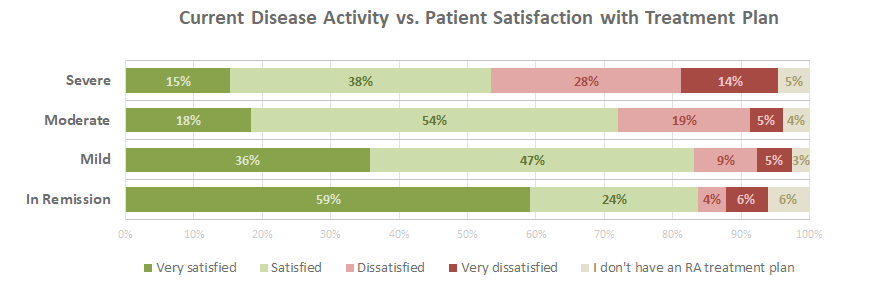
Results: The questionnaire was completed by 907 self-reported RA patients (90% women, 10% men), with a mean (SD) age of 58 years and a mean of 11.1 (10.1) years since diagnosis. According to self-reports, 5% were in remission, 22% reported mild DA, 54% moderate DA, and 19% severe DA. The majority (571; 63%) of patients were not asked by a provider about goals for their RA treatment. Of these, 32% were dissatisfied or very dissatisfied with their RA treatment plan, compared with only 13% of those who were asked about treatment goals.
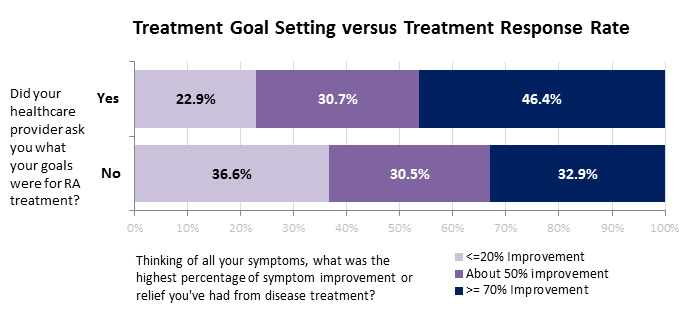
Patients not asked about RA treatment goals had DA improvement levels resembling those of the whole study population. However, those whose providers discussed goals with them were more likely to have more DA improvement. Of those who said they discussed goals, fewer had DA improvement levels of ≤20% (no, 23%; yes, 37%); and more had DA improvement levels ≥90% (no, 13%; yes 21%).
Those who did not discuss treatment goals with their provider were less likely to achieve remission than those who did not (4% and 7% respectively). Those discussing treatment goals were less likely to have severe DA (no, 21%; yes, 18%). When asked whether they were likely to use materials to help set treatment goals with providers, 79% were likely or very likely to use them. Patients with higher levels of DA improvement were as likely to prefer treatment goal setting materials as those with lower levels of improvement.
Conclusion: This web-based survey showed that most RA patients are not asked about their treatment goals by their providers. However, a majority of RA patients favor tools to help patients set treatment goals together with providers. Of those who are not asked to set goals, 75% report having moderate to severe DA. Further research should seek a broader understanding of patient preferences for treatment goals and how they relate to successful management of RA.
To cite this abstract in AMA style:
O'Neill K, Crowson C, Symons D, Sinicrope P, Myasoedova E, Bock M, Tilburt J, Davis J. Importance of Discussing RA Treatment Goals: Patients Report Providers Seldom Discuss Treatment Goals and Outcomes Improve When Goals Are Discussed [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/importance-of-discussing-ra-treatment-goals-patients-report-providers-seldom-discuss-treatment-goals-and-outcomes-improve-when-goals-are-discussed/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/importance-of-discussing-ra-treatment-goals-patients-report-providers-seldom-discuss-treatment-goals-and-outcomes-improve-when-goals-are-discussed/