Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Despite recognition that rheumatoid arthritis (RA) accelerates cardiovascular disease (CVD) and hypertension impacts 50% of RA patients, up to 50% lack blood pressure (BP) control, overlooking the most modifiable CVD risk factor. Rheumatology clinics record BP routinely but do not routinely manage it. As we previously reported, only 10% of RA clinic notes with high BP included follow-up recommendations. We subsequently reported that our adapted evidence-based BP Connect staff protocol doubled the odds of timely follow-up of high BPs and reduced population level BPs across three academic rheumatology clinics (Bartels et al. AC&R 2019). Preparing for wider dissemination, we sought to replicate our findings in a community rheumatology clinic setting.
Methods: We prospectively examined the feasibility and impact of our staff-based BP Connect protocol at a community rheumatology clinic using pre-post design. Pre-and post-protocol rates of primary care BP follow-up referrals were the primary outcome of electronic health record (EHR) data analysis. We first analyzed workflows through a focus group with clinic staff nurses, medical assistants, and schedulers to tailor protocols for the new clinic. Next, a one hour training was provided on rheumatologic CVD risk and BP, BP measurement skills review, protocol talking points, and EHR navigation. Two EHR alerts and monthly staff audit feedback supported implementation. Mid-implementation focus groups and questionnaires evaluated staff feasibility and acceptability.
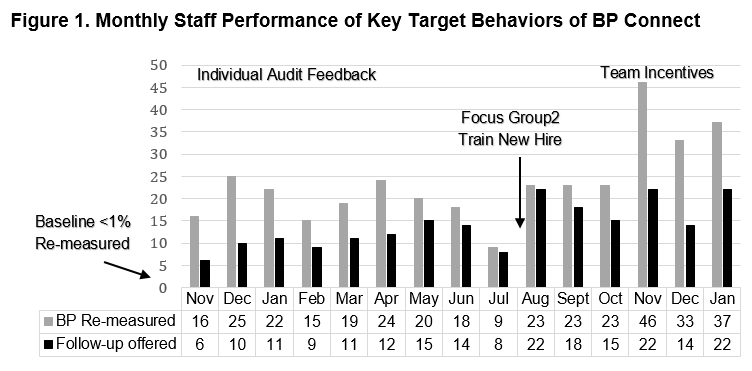
Results: Overall, compared to < 1% baseline remeasurement of high BPs in the rheumatology clinic, we reached two monthly peaks of 84%, and overall in 353 of 767 (46%) patients, high BP was re-measured post-implementation. Among 263 rheumatology patients with confirmed high BP re-measurement, 209 (79%) were offered follow-up for high BP, and among those, 109 (41%) accepted primary care follow-up (Table 1). After initial gains, a mid-implementation decline corresponded to clinic staff turnover and reduced staff-to-visit ratios. Increases in the last months occurred following focus group problem-solving, new hire training, and the introduction of modest team incentives based on clinic-level goals for staff performance (Fig 1).
Mixed methods findings included staff focus group and questionnaire responses. Rheumatology staff’s baseline usual practices followed three steps: (1) identifying high BP, (2) variable follow-up within the clinic, and (3) occasional follow-up across settings (i.e., primary care). Post-implementation, staff were satisfied with protocol support for these steps. Among six pre- and four post-implementation respondents, self-efficacy and confidence in perceived ability to do something to improve BP care increased from 3.8 to 4.5 on a 5-point Likert scale.
Conclusion: Replicating the implementation of the BP Connect systems-based staff protocol in a community rheumatology clinic improved primary care follow‐up referrals for high BP. Findings highlight a scalable strategy to improve BP follow‐up and rheumatology population health and new findings regarding the potential role of team-based incentives.
To cite this abstract in AMA style:
Ramly E, White D, Perez A, Bartels C. Implementing the BP Connect Systems-Based Blood Pressure Follow-Up Protocol with Community Rheumatology Clinic Teams [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/implementing-the-bp-connect-systems-based-blood-pressure-follow-up-protocol-with-community-rheumatology-clinic-teams/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implementing-the-bp-connect-systems-based-blood-pressure-follow-up-protocol-with-community-rheumatology-clinic-teams/