Session Information
Date: Tuesday, October 23, 2018
Title: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
The delivery of osteoporosis services is sub-optimal nationally and throughout the Veterans Affairs (VA) healthcare system and particularly poor for rural Veterans. To meet this critical need, we developed a Rural Bone Health Team (BHT), to provide efficient, evidence-based primary prevention osteoporosis services to rural Veterans. We compared the proportion of osteoporosis screening and treatment in Veterans choosing to participate and those who did not participate, both before and after the establishment of the BHT.
Methods:
To identify Veterans with osteoporosis risk factors, we operationalized evidence-based screening guidelines into queries to the VHA Corporate Data Warehouse (CDW), a repository of medical and pharmacy records. Captured risk factors included Osteoporosis Self-assessment Tool (OST) score, sex, age, and/or chronic exposure to high risk medications. Veterans at risk were sent enrollment letters, invited to receive care by the BHT, and on acceptance evaluated by clinical nurse educators via standard protocols. As appropriate, enrolled Veterans received DXA scans, education on bone healthy lifestyle, additional fracture risk assessment, and triage for treatment if identified as either osteoporosis or high-risk osteopenia. Advanced practice providers then evaluated Veteran’s need for osteoporosis pharmacotherapy, performed laboratory evaluations for secondary causes of bone loss, discussed risks/benefits of pharmacological therapies, and when indicated, therapy initiated and monitored therapy at scheduled intervals. For this study, we included Veterans contacted by the Rural BHT between 12/1/2016 and 02/01/2018. A non-experimental cohort design was utilized to assess pre-specified outcome and process measures, including the number of Veterans contacted, Veterans electing enrollment, DXAs completed, and Veterans receiving pharmacological therapy.
Results:
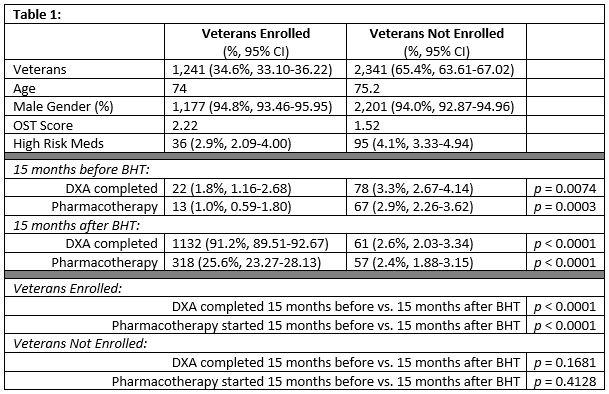
During the first 15 months of implementation, the Rural BHT contacted 3,582 Veterans, with 1,241 (34.6%) Veterans accepting enrollment and 1,132 (91.2%) enrollees completing a DXA scan. Of those participating Veterans, 318 (25.6%) met criteria for and accepted pharmacological therapy. As illustrated in the Table Veterans choosing to participate in the Rural BHT were significantly more likely to complete a DXA scan (91.2% vs. 2.6%, p < 0.0001) and to receive pharmacological therapy (25.6% vs. 2.4%, p < 0.0001) than those choosing not to participate.
Conclusion:
Enrollment in the Rural BHT significantly increases the likelihood that rural Veterans will received appropriate screening and treatment for osteoporosis. This model for the delivery of primary prevention services for osteoporosis provides unique processes and procedures without adding workload to the primary care team and could potentially be adapted to provide other preventative services, as well as instituted in other care settings outside VA.
To cite this abstract in AMA style:
Miller KL, Patel S, Cannon GW, Anderson ZL. Implementation of a Primary Prevention, Population-Based Virtual Osteoporosis Clinic Dramatically Increases the Number of Rural Veterans Receiving Osteoporosis Screening and Treatment [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/implementation-of-a-primary-prevention-population-based-virtual-osteoporosis-clinic-dramatically-increases-the-number-of-rural-veterans-receiving-osteoporosis-screening-and-treatment/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implementation-of-a-primary-prevention-population-based-virtual-osteoporosis-clinic-dramatically-increases-the-number-of-rural-veterans-receiving-osteoporosis-screening-and-treatment/