Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Myocardial
microvascular dysfunction may precede or coexist with coronary atherosclerosis
and heart failure, two conditions over-represented in RA. Coronary
flow reserve (CFR) offers an indirect index of myocardial microvascular
function. We investigated indicators of CFR and its association
with cardiac structure and function in RA.
Methods: RA patients without known cardiovascular disease
underwent 13N-ammonia
cardiac positron emission tomography (PET) vasodilator myocardial perfusion
imaging to evaluate myocardial ischemia and CFR. Global myocardial
blood flow (MBF) was quantified at rest and during peak hyperemia
with CFR=peak stress MBF/rest MBF, Participants also underwent 3-D echocardiography
to assess left ventricular (LV) mass, volumes, and systolic and diastolic
function. Mass and volume measures were indexed to height. Generalized linear
models were used to explore the associations of patient characteristics with CFR,
and measures of LV structure and function.
Results: A total of 76 RA patients [mean age=54 yrs;
80% Female; 43% and 36% non-Hispanic White and Hispanic, respectively; Median
RA duration=7.1 yrs; 70% RF or anti-CCP positive; mean DAS28=3.6; 39% treated
with biologics] were analyzed. Mean ± SD CFR was 2.9 ± 0.8, and 12% had a
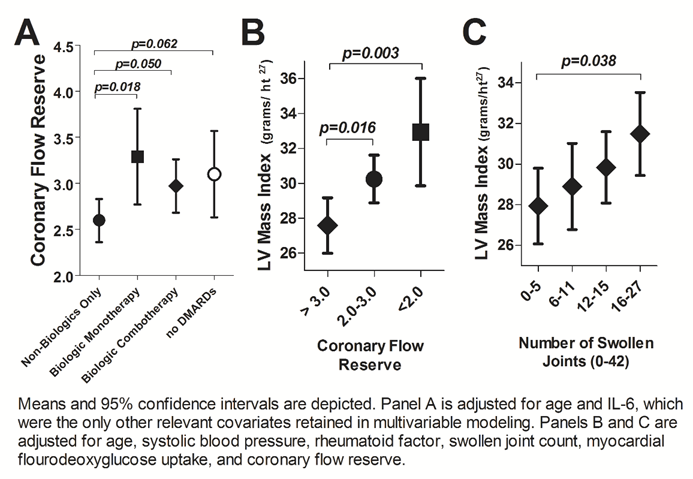
CFR<2.0 (an established abnormal threshold). After adjustment, male sex,
IL-6, and non-biologic DMARD use were significantly and inversely associated
with CFR, while biologic use was associated positively. On average, CFR was
lower by 0.18 units for every log unit higher IL-6 (p=0.022). Adjusting for
sex and IL-6, RA patients treated with only non-biologics had significantly
lower CFR compared with those treated with any biologics or no DMARDs (Fig 1.a).
Associations were maintained after adjusting for coronary macrovascular disease
[i.e. coronary artery calcification (CAC)]. CFR was not associated with
diabetes, smoking, prednisone use, or lipids in adjusted models. Adjusting for
relevant demographic and CVD risk factors, CFR<2.0 was associated with a 5.4
unit higher LV mass index (p=0.003; Fig 1.b), the equivalent of 60 mm Hg higher
systolic blood pressure (SBP). In the same model, each swollen joint, on
average, was associated with a 0.16 unit higher LV mass index (p=0.038),
equivalent to almost 2 mm Hg higher SBP, per joint (Fig 1.c). Lower CFR was
also significantly associated with higher LV end-diastolic and systolic
volumes, but there was no significant association with ejection fraction or
measures of diastolic dysfunction.
Conclusion: Higher IL-6 and non-treatment with
biologics were among the strongest indicators of lower CFR, which, along with
higher swollen joint counts, was associated with higher LV mass. These data
suggest that articular and systemic inflammation may contribute to the
microvascular and myocardial structural changes in RA that are known to precede
heart failure.
To cite this abstract in AMA style:
Amigues I, Giles JT, Bokhari S, Zartoshti A, Weinberg R, Russo C, Bathon J. Impaired Coronary Flow Reserve in Rheumatoid Arthritis: A Robust Indicator of Cardiac Structure Associated with Systemic Inflammation and Rheumatoid Arthritis Treatments [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/impaired-coronary-flow-reserve-in-rheumatoid-arthritis-a-robust-indicator-of-cardiac-structure-associated-with-systemic-inflammation-and-rheumatoid-arthritis-treatments/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impaired-coronary-flow-reserve-in-rheumatoid-arthritis-a-robust-indicator-of-cardiac-structure-associated-with-systemic-inflammation-and-rheumatoid-arthritis-treatments/