Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Lupus nephritis (LN) affects up to 40% of patients with SLE and leads to end stage kidney disease (ESKD) in 17-33% after 10 years. The prevalence of chronic kidney disease stage IV (estimated glomerular filtration rate, eGFR=15-29ml/min/1.73m2) is not known; however, approximately two thirds of such patients will progress to ESKD after 6 years on average.1
Objective: To determine the impact of time to remission and flares on the development of advanced CKD (stage IV or worse) in LN.
Methods: Patients with LN based on biopsy or abnormal proteinuria ( >0.5g/day) with or without hematuria/pyuria/casts for two consecutive visits in the absence of other plausible explanation were retrieved from the Toronto Lupus Clinic database. Individuals with advanced CKD at baseline were excluded. All patients were followed for at least 5 years. The primary outcome was the development of advanced CKD (eGFR≦29ml/min/1.73m2). Remission was defined as proteinuria< 0.5g/24h, no active urinary sediment and serum creatinine of £120% of baseline. Flare was defined as any abnormal proteinuria ( >0.5g/day) after remission. Death was treated as competing risk in survival analysis. Statistical analysis with SAS 9.4; p< 0.05 was considered significant.
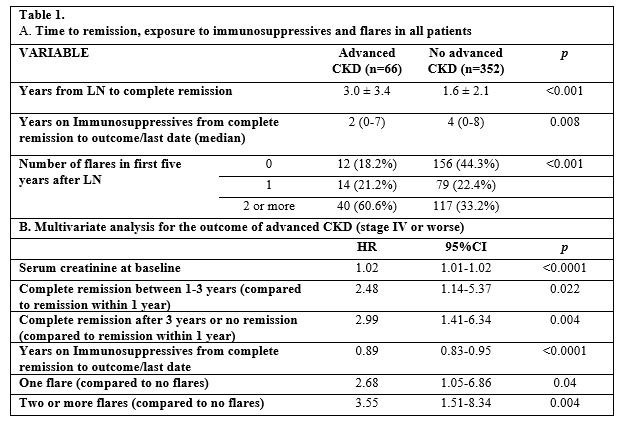
Results: Out of 418 eligible patients, 209 (50%) achieved remission within the first year from LN diagnosis, 102 (24.4%) within the 2nd and 3rd years, 70 (16.7%) after 3 years and 37 (8.9%) never achieved remission. Sixty-six patients (15.8%) developed advanced CKD after 9.5 years on average (37 with ESKD). At baseline, these patients had a higher SLICC/Damage Index (0.6±1.2 vs. 0.3±0.7, p=0.003), lower eGFR (73±38 vs. 94±33ml/min/1.73m2, p< 0.001), higher prevalence of hypertension (85% vs. 73%, p=0.046), proliferative nephritis (combined class III and IV, 66% vs. 47.8%, p=0.017) and more often treated with ACE inhibitors or angiotensin receptor blockers (35% vs. 22%, p=0.02). The other variables did not differ significantly. Remission rates, flares and exposure to immunosuppressives after remission are shown in Table 1.
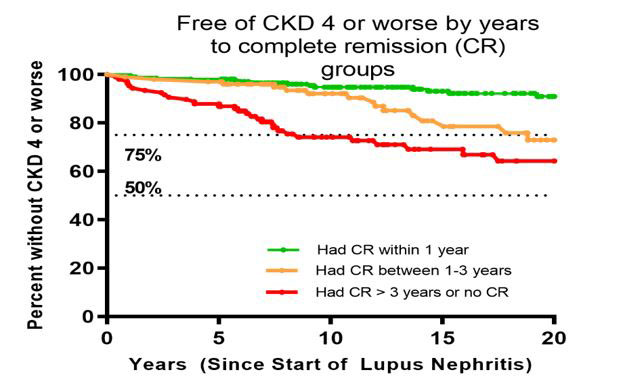
Patients who achieved remission within one year from diagnosis demonstrated better outcomes compared to all other groups (p< 0.0001), Figure 1. Patients with complete remission between one and three years had similar outcomes for the first 10 years from diagnosis and deteriorated during the second decade of follow-up.
Conclusion: Complete remission within the 1st year from LN diagnosis strongly protects against advanced CKD. Flares significantly affect prognosis. One flare was associated with 2.7-fold increased risk for advanced CKD (3.6-fold for 2 or more flares). Longer time on immunosuppressives after remission is associated with decreased risk for advanced CKD. Our findings emphasize the importance of early remission as well as flare prevention with prolonged immunosuppressive use to maximize renal survival in LN.
To cite this abstract in AMA style:
Gladman D, TSELIOS K, Su J, Urowitz M. Impact of Time to Remission, Flares and Exposure to Immunosuppressives on the Development of Advanced Chronic Kidney Disease (Stage IV or Worse) in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/impact-of-time-to-remission-flares-and-exposure-to-immunosuppressives-on-the-development-of-advanced-chronic-kidney-disease-stage-iv-or-worse-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-time-to-remission-flares-and-exposure-to-immunosuppressives-on-the-development-of-advanced-chronic-kidney-disease-stage-iv-or-worse-in-lupus-nephritis/