Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Several studies showed lower socioeconomic status (SES) was associated with higher disease activity and lower quality of life (QOL) in patients with rheumatoid arthritis (RA). However, health insurance system may influence the association between SES and disease outcomes. Because Japan has the unique national insurance system, all Japanese citizens are required to be enrolled in the national insurance system. In addition, most patients pay 30 % of medical cost whereas patients aged 70 and older, patients with low income and patients with disabilities pay 0 to 20 % of cost depending on age, income and severity of disabilities. The impact of SES on RA disease outcomes in the Japanese health system is still unknown because it has never been examined in a Japanese cohort. It is also important for policymakers in other countries to refer to Japanese findings when they make or improve their health insurance system. We evaluated the effect of SES among Japanese patients with RA on disease activity, activities of daily living (ADL) and QOL in the Japanese national health insurance system.
Methods: A questionnaire survey was conducted among 339 patients with RA in Kobe University Hospital. Clinical characteristics included age, sex, disease duration, Steinbrocker stage and class classification, rheumatoid factor, anti-citrullinated protein antibody, use of corticosteroid, methotrexate, and biologic. Disease activity was assessed according to the DAS28-CRP, ADL according to the Japanese version of the Health Assessment Questionnaire (HAQ), and QOL according to the Japanese version of the EQ-5D. SES included income, education level and occupation. Univariate and multivariate analyses were conducted to examine the association of SES with DAS28-CRP, HAQ and EQ-5D. Because proportion of biologic use and self-pay were assumed as the intermediate variables between SES and disease outcomes, we evaluated whether they were associated with SES to investigate the possible mechanism through which SES affected disease outcomes.
Results: Univariate analyses showed patients with lower income had significantly higher DAS28-CRP (P = 0.03) and HAQ score (P = 0.001). Although education level was not associated with DAS28-CRP, HAQ or EQ-5D, patients with occupation had lower HAQ score than patients without (P < 0.001). Multivariate analyses adjusted for the confounders revealed the similar results (Figure). Although patients with lower income had lower proportion of self-pay (P < 0.001), lower income was associated with lower proportion of biologic use.
Conclusion: SES may influence disease activity and ADL among patients with RA in Japan. Although Japanese health insurance system successfully decreased self-pay among patients with lower income, it did not have enough effectiveness to increase the proportion of biologic use among such patients. More efforts are needed to solve equity issue. 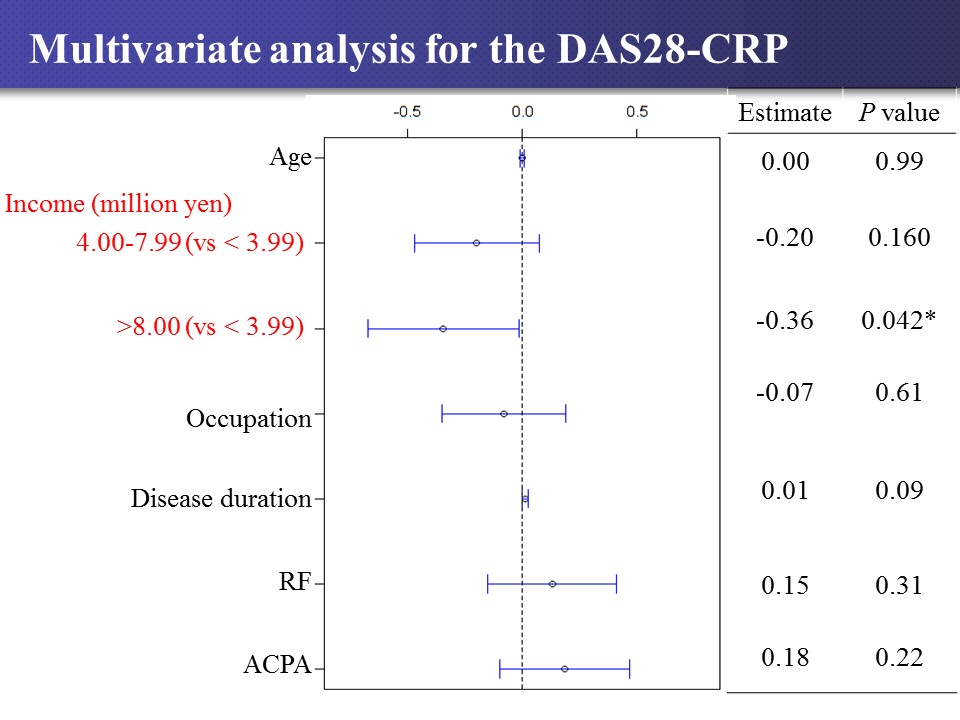
To cite this abstract in AMA style:
Onishi A, Kageyama G, Ueda Y, Naka I, Tsuda K, Okano T, Takahashi S, Akashi K, Sendo S, Kogata Y, Saegusa J, Morinobu A. Impact of Socioeconomic Status on Disease Outcomes in Japanese Patients with Rheumatoid Arthritis Under the Japanese National Insurance System [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/impact-of-socioeconomic-status-on-disease-outcomes-in-japanese-patients-with-rheumatoid-arthritis-under-the-japanese-national-insurance-system/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-socioeconomic-status-on-disease-outcomes-in-japanese-patients-with-rheumatoid-arthritis-under-the-japanese-national-insurance-system/
