Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) is a chronic autoimmune disease driven by T- and B-cell activation and pro-inflammatory cytokines such as TNF-α and IL-6 and is managed by disease-modifying antirheumatic drugs (DMARDs) [1]. SGLT2 inhibitors and GLP-1 receptor agonists, developed for type 2 diabetes, have shown cardiovascular, renal, and potential anti-inflammatory benefits via reduced cytokine production and macrophage activation [2-5]. Clinical data on their effect in RA is limited. This study examines the association between SGLT2 or GLP-1 use and RA flare outcomes in DMARD-treated patients using real-world retrospective data.
Methods: A retrospective cohort study was conducted using TriNetX data between 2019 and 2024. Adults with RA and >12 months follow-up after DMARD initiation were included and categorized into: (1) DMARDs only, (2) DMARDs + SGLT2 inhibitor, and (3) DMARDs + GLP-1 receptor agonist. Patients with other inflammatory arthritides, malignancy, transplant, pregnancy, combined SGLT2/GLP-1 use, or prolonged prednisone use ( >3 months) were excluded. Data included demographics, comorbidities, treatment timing, short-term oral prednisone, IV methylprednisolone, joint injections, ESR/CRP, and DMARD changes. RA flares were defined using a composite of: IV methylprednisolone, intra-articular injection, oral prednisone use less than 3 months, number of DMARD escalation, or increased CRP (≥10 mg/L) or ESR (≥20 mm/h).
Results: In Table 1, the GLP-1 group had the highest baseline DMARD count (mean 2.51), lowest end count (mean 1.31). ESR and CRP were most elevated in the SGLT2i group. Table 2 reports significantly different flare burden scores (p = 0.00006): DMARDs-only (1.12 ± 2.44), DMARDs+GLP-1 (1.71 ± 3.79), and DMARDs+SGLT2i (1.30 ± 1.78). Flare proxies such as IV steroids, joint injections, and inflammatory marker elevations were more common in the GLP-1 group. The composite flare burden score included oral prednisone use (1 point if present), IV methylprednisolone and joint injections (1 point per three administrations), frequency of CRP ≥10 mg/L, frequency of ESR ≥20 mm/hr, and if DMARD escalation was present. Flare proxies like IV steroids, injections, and inflammatory marker elevations were more frequent in the GLP-1 group. These findings suggest a possible association between GLP-1 use and higher flare burden, though further adjustment for baseline differences is needed. Table 3 shows patients with post-initiation flare declined significantly in the SGLT2i group (34.1% to 12.0%, p = 0.0407) and non-significantly in the GLP-1 group (41.0% to 20.7%, p = 0.1525). Limitations include lack of standardized disease activity measures (e.g., DAS28), potential confounding factors, and the inability to include DMARD escalation in pre-treatment and post-treatment analysis.
Conclusion: The use of SGLT2i was associated with a significant reduction in RA flares. GLP-1 showed a non-significant trend toward flare reduction, though this may reflect higher baseline RA severity which may influence the trend. These findings support the need for further prospective studies to validate the anti-inflammatory potential of SGLT2 inhibitors in RA and further explore the effect of GLP-1 on RA flare.
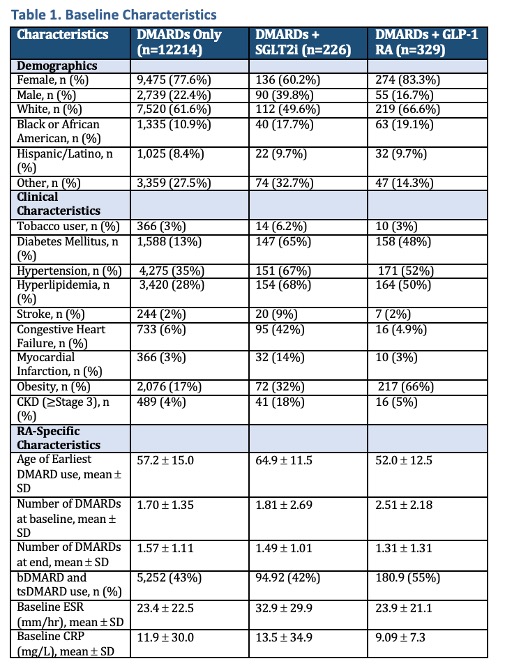 This table compares demographics, clinical comorbidities, and RA-specific characteristics among patients on DMARDs only, DMARDs + SGLT2 inhibitors, and DMARDs + GLP-1 receptor agonists.
This table compares demographics, clinical comorbidities, and RA-specific characteristics among patients on DMARDs only, DMARDs + SGLT2 inhibitors, and DMARDs + GLP-1 receptor agonists.
.jpg) This table shows the number of patients in each group who experienced flare-related events. The RA Flare Composite Score was calculated per patient to reflect total flare burden: 1 point each for oral prednisone use, elevated CRP (≥10 mg/L), elevated ESR (≥20 mm/h), and DMARD escalation; IV steroids and joint injections counted as 1 point per three counts. Higher scores reflect more flare activity.
This table shows the number of patients in each group who experienced flare-related events. The RA Flare Composite Score was calculated per patient to reflect total flare burden: 1 point each for oral prednisone use, elevated CRP (≥10 mg/L), elevated ESR (≥20 mm/h), and DMARD escalation; IV steroids and joint injections counted as 1 point per three counts. Higher scores reflect more flare activity.
.jpg) This table shows the number and percentage of patients who experienced a flare before and after starting GLP-1 receptor agonists or SGLT2 inhibitors.
This table shows the number and percentage of patients who experienced a flare before and after starting GLP-1 receptor agonists or SGLT2 inhibitors.
To cite this abstract in AMA style:
Sakthivel S, Karpman M, Oland L, Aldamouk A. Impact of SGLT2 Inhibitors and GLP-1 Agonists on RA Flares in Patients on DMARD Therapy: A Retrospective Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-sglt2-inhibitors-and-glp-1-agonists-on-ra-flares-in-patients-on-dmard-therapy-a-retrospective-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-sglt2-inhibitors-and-glp-1-agonists-on-ra-flares-in-patients-on-dmard-therapy-a-retrospective-study/
