Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Atrial Fibrillation (AF) is a common cardiac arrhythmia related to increased cardiovascular morbidity and mortality. There is a significant association of systemic inflammation with the pathogenesis of AF. Several studies have assessed the relationship of AF with Rheumatoid Arthritis (RA) with variable results. Some studies suggest 29-40% higher incidence of AF with RA, while others did not find any increased risk of AF in RA. In this study, we used the National Inpatient Sample (NIS) to assess the impact of RA on demographics, mortality, length of stay, and cost per hospitalization for AF in comparison to non-RA hospitalizations.
Methods: Healthcare Cost and Utilization Project’s NIS is the largest all-payer inpatient database in the United States with discharge data from >1200 hospitals, located across the nation. We queried the National Inpatient Sample from 2010-2014 to identify adult hospitalizations for AF with and without RA, using validated ICD-9 CM codes. Logistic regression analysis was used to identify independent associations with in-hospital mortality. Multivariate regression was applied to adjust for confounders.
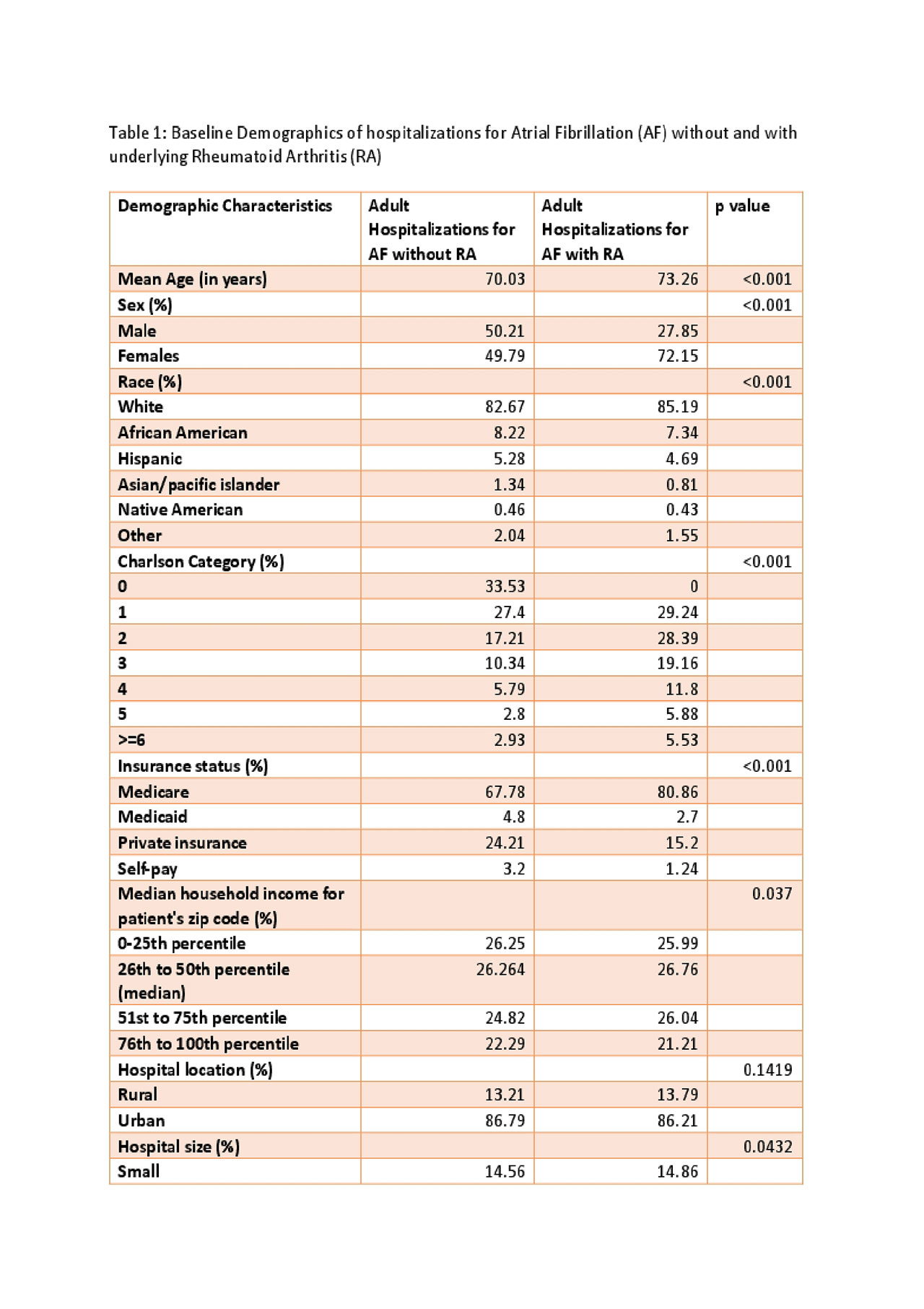
Results: There were an estimated 43910 adult hospitalizations for AF with a secondary diagnosis of RA, from 2010 to 2014. On univariate analysis, the average age for hospitalizations with AF in the non-RA group was 70.03years, whereas, in the RA group, the average age for was 73.26 years (p< 0.001). 72.15% of all hospitalizations with AF & RA were females (significantly higher, p-value < 0.001). Unadjusted logistic regression suggested an increased risk of mortality in patients with AF & RA with an odds ratio of 1.297 (p value=0.01), but after adjusting for confounders, a relative decrease in mortality was identified patients with AF & RA (Adjusted Odds Ratio=0.781; p value=0.025). Unadjusted Linear regression for length of stay (LOS) per hospitalization suggested longer length of stay for patients with AMI & RA (3.837 days vs. 3.41 days, p-value < 0.001), but when adjusted for confounders with multivariate regression, LOS was found to be lower (Coefficient = -0.243; p value< 0.001)
Conclusion: This study reports contemporary data of AF & RA hospitalizations over five years in the United States. It suggests that patients with AF and RA have similar and possibly better outcomes for mortality compared to the non-RA population when adjusted for confounding factors like age, gender, and other demographic factors. Further prospective studies are needed to understand the relationship between AF and RA.
To cite this abstract in AMA style:
Jatwani S, Chugh K, Bindra B, Jatwani K. Impact of Rheumatoid Arthritis on Outcomes of Atrial Fibrillation: Results for National Inpatient Sample [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-on-outcomes-of-atrial-fibrillation-results-for-national-inpatient-sample/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-on-outcomes-of-atrial-fibrillation-results-for-national-inpatient-sample/