Session Information
Date: Monday, November 11, 2019
Title: Metabolic & Crystal Arthropathies Poster II: Clinical Trials & Basic Science
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Increased serum uric acid (sUA), hyperuricemia, has been reported to be associated with psoriasis (1). Increased cell turnover in psoriatic skin lesions has been proposed as a potential mechanism, but results are conflicting (1). In this study we assessed levels of sUA to degree and severity of skin involvement measured by Psoriasis Area Severity Index (PASI) at baseline and after treatment with the IL-17A inhibitor, secukinumab. The objectives were to adress the following questions: 1) are PASI and sUA levels correlated; and 2) are changes in PASI associated with changes in sUA during treatment of psoriasis.
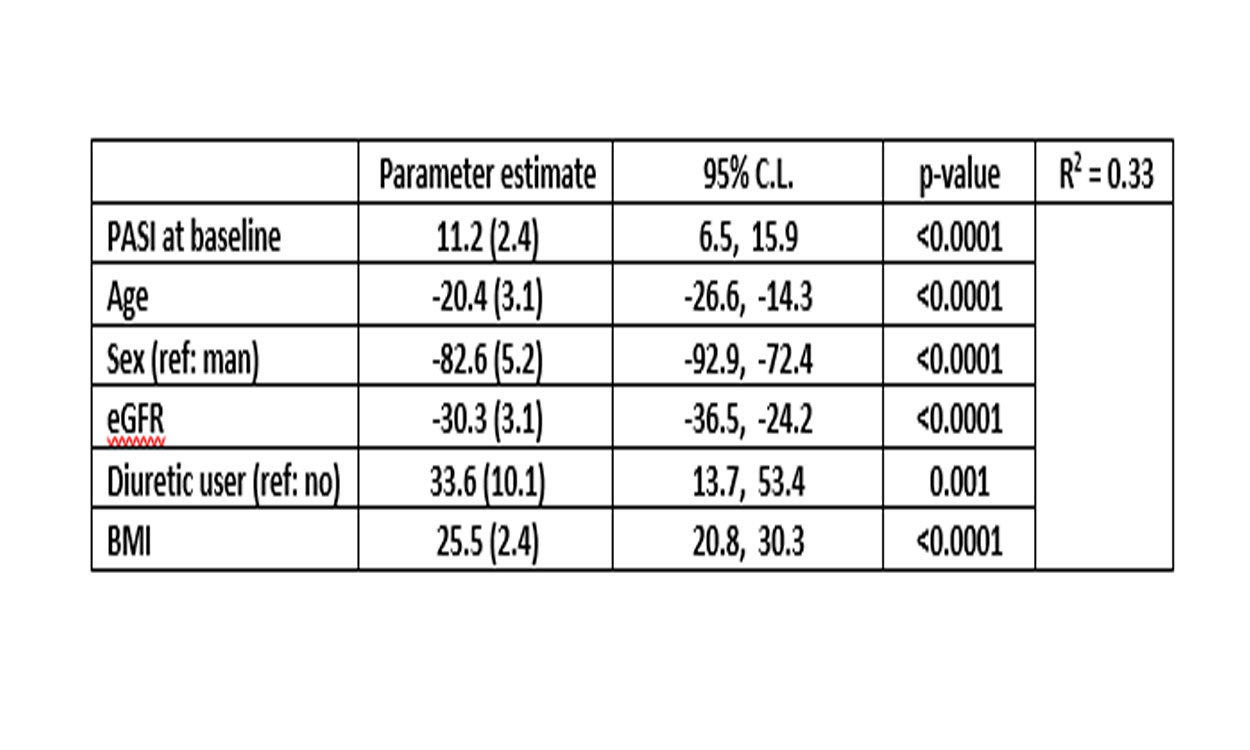
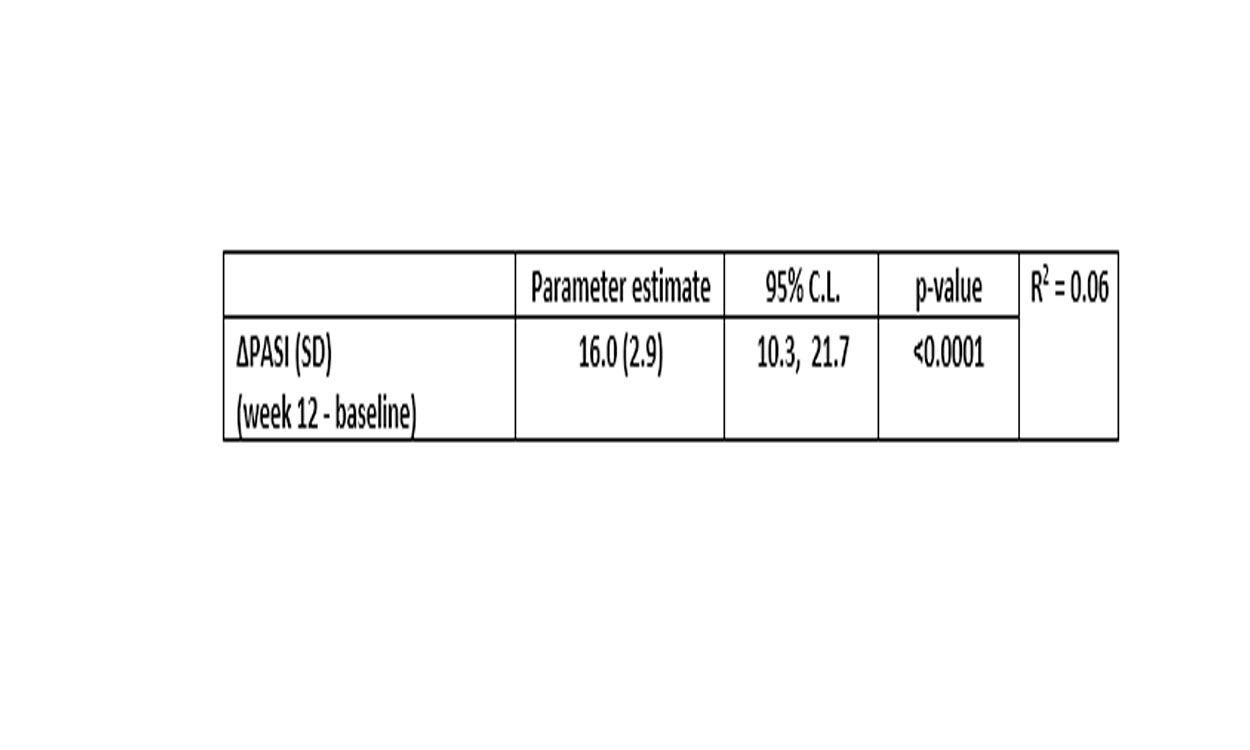
Methods: Subjects with psoriasis/psoriatic arthritis (N=1042/204 (19.6%)) with concomitant psoriatic arthritis in three RCTs (ERASURE, FIXTURE and SCULPTURE) treated with secukinumab (dose 300 mg, n=628) or placebo (n=414) were pooled and included. At baseline values for sUA and PASI and the following co-variates were assessed; age, sex, BMI, renal function defined as eGFR, medication with diuretics (%), these are all variables known to affect sUA levels. To assess change in PASI (ΔPASI) and sUA (ΔsUA) the differences (week 12 minus baseline) in subjects receiving active drug were used. Multivariable linear regression, adjusting for identified co-variates, was used to assess the association between PASI and sUA at baseline with all subjects pooled and to assess the association between ΔsUA and ΔPASI over 12 weeks intervention in only those treated with secukinumab. All continuous variables were standardized with the exception of the dependent variable sUA, hence an increase in parameter estimates represent the change in sUA per 1 standard deviation (at baseline) difference in PASI and other continuous co-variates.
Results: Baseline characteristics; 70% were male, 6% were on diuretics and mean (SD) age, BMI and e GFR were 45 (13) yrs, 29.2 (6.8) kg/m2 and 96 (17) mL/min/1.73m2, respectively. From baseline to week 12, in patients treated with secukinumab, mean (SD) PASI decreased from 23.7 (SD: 10) to 2.9 (SD: 5) and sUA from 366 (SD: 96) to 359 (SD: 94) µmol/L. At baseline, covariates explained 33% of the variance in sUA with a significant contribution of PASI. A higher PASI value of 1 SD (10 units) was associated with 11.2 (p >0.0001) µmol/L higher value of sUA in the fully adjusted model. Other co-variates had larger effects (table 1). During 12 week follow-up, co-variates explained little of the variation in ΔsUA (R2=0.06), but there was a significant association with ΔPASI (Table 2) in fully adjusted model.
Conclusion: Both the degree and change in skin involvement in psoriasis were modestly associated with sUA, supporting a potential pathophysiological relationship. Known risk factors for sUA had however a larger impact cross-sectionally. Furthermore, sUA decreased modestly with 12 week treatment with secukinumab.
Ref
- Li X, Miao X, Wang H, Wang Y, Li F, Yang Q, et al. Association of serum uric acid levels in psoriasis: A systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e3676.
To cite this abstract in AMA style:
Dehlin M, Fasth A, Reinhardt M, Jacobsson L. Impact of Psoriasis Disease Activity and Other Risk Factors on Serum-urate Levels in Patients with Psoriasis and Psoriatic Arthritis – A Post-hoc Analysis of Pooled Data from Three Phase 3-trials with Secukinumab [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-psoriasis-disease-activity-and-other-risk-factors-on-serum-urate-levels-in-patients-with-psoriasis-and-psoriatic-arthritis-a-post-hoc-analysis-of-pooled-data-from-three-phase-3-trials-with/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-psoriasis-disease-activity-and-other-risk-factors-on-serum-urate-levels-in-patients-with-psoriasis-and-psoriatic-arthritis-a-post-hoc-analysis-of-pooled-data-from-three-phase-3-trials-with/