Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Autoimmune cytopenias may precede or occur with childhood-onset systemic lupus erythematosus (cSLE). Adult studies suggest that lupus patients with concurrent autoimmune cytopenias have relatively lower prevalence of lupus nephritis (LN) and are a unique disease sub-population. The reason for this association is unclear. Also, it has not been well studied in cSLE which has a higher risk of LN. LN often occurs within 2 years of cSLE diagnosis. Since autoimmune cytopenias are more common in cSLE and often occur early in this disease, assessing their impact on cSLE phenotype is important. In addition, the effect of treatment for idiopathic autoimmune cytopenias on subsequent cSLE has not previously been explored. Therefore, the objectives of our study were to assess whether in cSLE, autoimmune cytopenias decrease the 2-year risk and severity of LN; to assess associated serologic differences in those with and without autoimmune cytopenias at cSLE diagnosis; the effect of prior immune therapy for autoimmune cytopenias on 2-year risk of LN; and to perform descriptive analyses of these pediatric patients without LN at cSLE diagnosis.
Methods: We conducted a retrospective cohort study of incident cSLE cases at our institution from January 1, 2000 to June 30, 2016. We included patients aged less than 17 years who met American College of Rheumatology and/or Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. We excluded patients diagnosed outside our institution and those with LN at cSLE diagnosis. Our follow-up period was 2 years. We defined autoimmune cytopenias as either autoimmune hemolytic anemia, Coombs positive anemia without hemolysis, immune thrombocytopenia or Evan’s syndrome before or at cSLE diagnosis.
Results: We had 130 incident cSLE patients who met our inclusion and exclusion criteria. Of these, 43 (33%) had autoimmune cytopenias (Figure1). At cSLE diagnosis, there was no serologic difference between those with and without autoimmune cytopenias. Those with autoimmune cytopenias had significantly more neuropsychiatric symptoms and higher mean ESR versus those without autoimmune cytopenias. However, they had less arthritis, malar rash and myositis (Table1). 2-year incidence of LN was 12% in our cohort. Patients with autoimmune cytopenias had lower 2-year risk of LN compared to other cSLE patients (7% vs 15%). Of the 16 patients that developed LN, those with autoimmune cytopenias had mostly class V (2 of 3 patients) versus mostly class III and IV in those without autoimmune cytopenias (6 of 12 patients). None of the 13 patients pre-treated for autoimmune cytopenias prior to cSLE diagnosis developed LN.
Conclusion: Patients with autoimmune cytopenias before or at cSLE diagnoses have statistically significant and clinically relevant differences in their presentation from other cSLE patients. Our findings call for further studies on the immunologic and genetic basis of these differences.
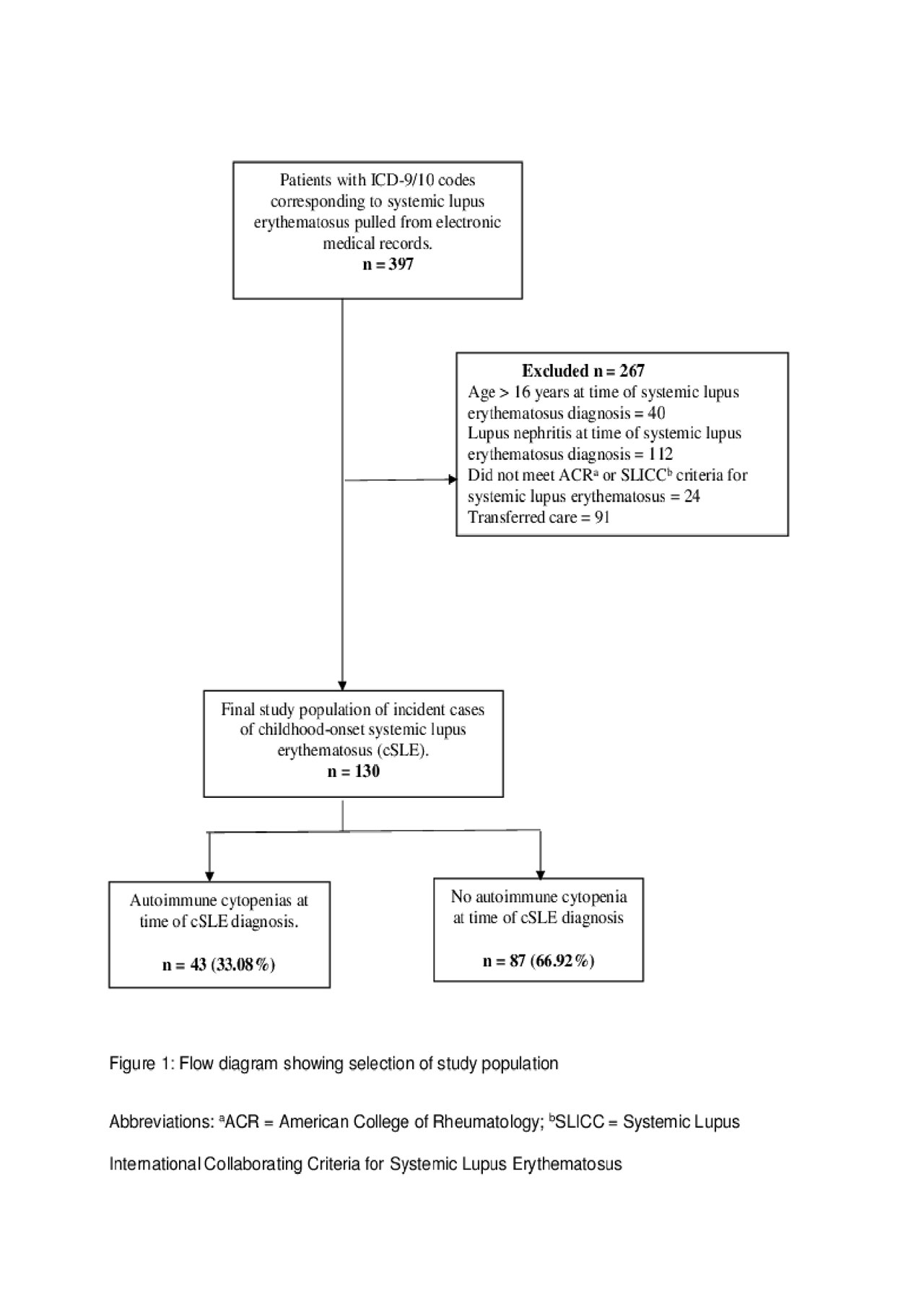
Ogbu – ACR 2019 submission – Images
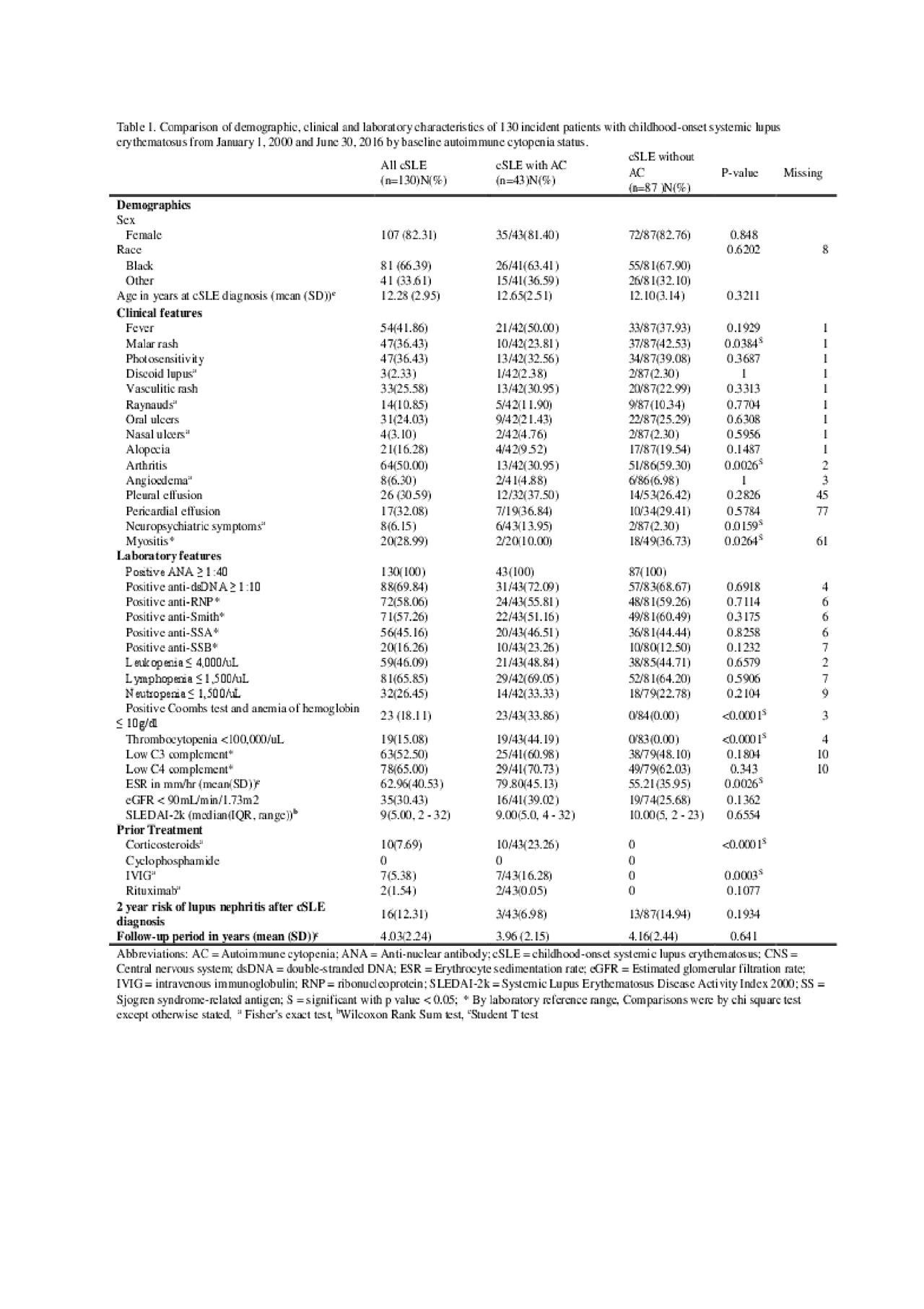
Ogbu – ACR 2019 submission – Table 1
To cite this abstract in AMA style:
Ogbu E, Chandrakasan S, Rouster-Stevens K, Greenbaum L, Marion C, Singer K, Sanz I, Prahalad S. Impact of Preceding and Co-existing Autoimmune Cytopenias on Severity of Childhood-onset Systemic Lupus Erythematosus: A Single-Center Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-preceding-and-co-existing-autoimmune-cytopenias-on-severity-of-childhood-onset-systemic-lupus-erythematosus-a-single-center-retrospective-cohort-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-preceding-and-co-existing-autoimmune-cytopenias-on-severity-of-childhood-onset-systemic-lupus-erythematosus-a-single-center-retrospective-cohort-study/
